Fun fact: there is no rheumatological Diagnostic Criteria, says the American College of Rheumatology.
Your rheumatologist's diagnosis, or lack thereof, is the "Gold Standard."

Thud. That’s the sound my heart made when I read this 2015 article from the American College of Rheumatology (ACR). This detour, from multiple autoimmune syndrome, into Diagnostic Classification, started when I was checking the classifications the latest study was using for Sjogren’s Syndrome. The most up-to-date classification for Sjogren’s Syndrome can be found here. I didn’t understand that the American College of Rheumatology and their international partner organization, the European League Against Rheumatism, was defining Classification Criteria differently from Diagnostic Criteria.
What is Diagnostic Criteria?
Diagnostic criteria is typically a number-weighted set of signs and symptoms associated with a disease. You get a certain score based on the number assigned to each area, and if your score is equal to or above a certain number, you are considered to have the disease. Many diseases do not have professional and scientific consensus on diagnostic criteria, but I thought that many of the better known and studied autoimmune disorders would have diagnostic criteria. As far as rheumatological autoimmune disorders go, I was wrong.
The benefits of diagnostic criteria are clear. They are usually as well-researched and well-validated as possible, drawing on the most up-to-date scientific knowledge and consensus of a wide range of experts in the field. Diagnostic criteria standardizes a diagnosis nationally, and sometimes internationally. Ideally, it helps clinicians avoid misdiagnosis. Diagnostic criteria can help to characterize the actual prevalence of a disease in a society. An accurate diagnosis is important because it provides direction for effective treatment. It’s also an empowering validation tool for the person suffering from autoimmune symptoms—it’s a way to check your rheumatologist’s clinical work up and diagnostic conclusions. For the patient, diagnostic criteria has the potential to limit the man-behind-the-curtain, Wizard of Oz, odysseys that plague autoimmune symptom sufferers.
The Article
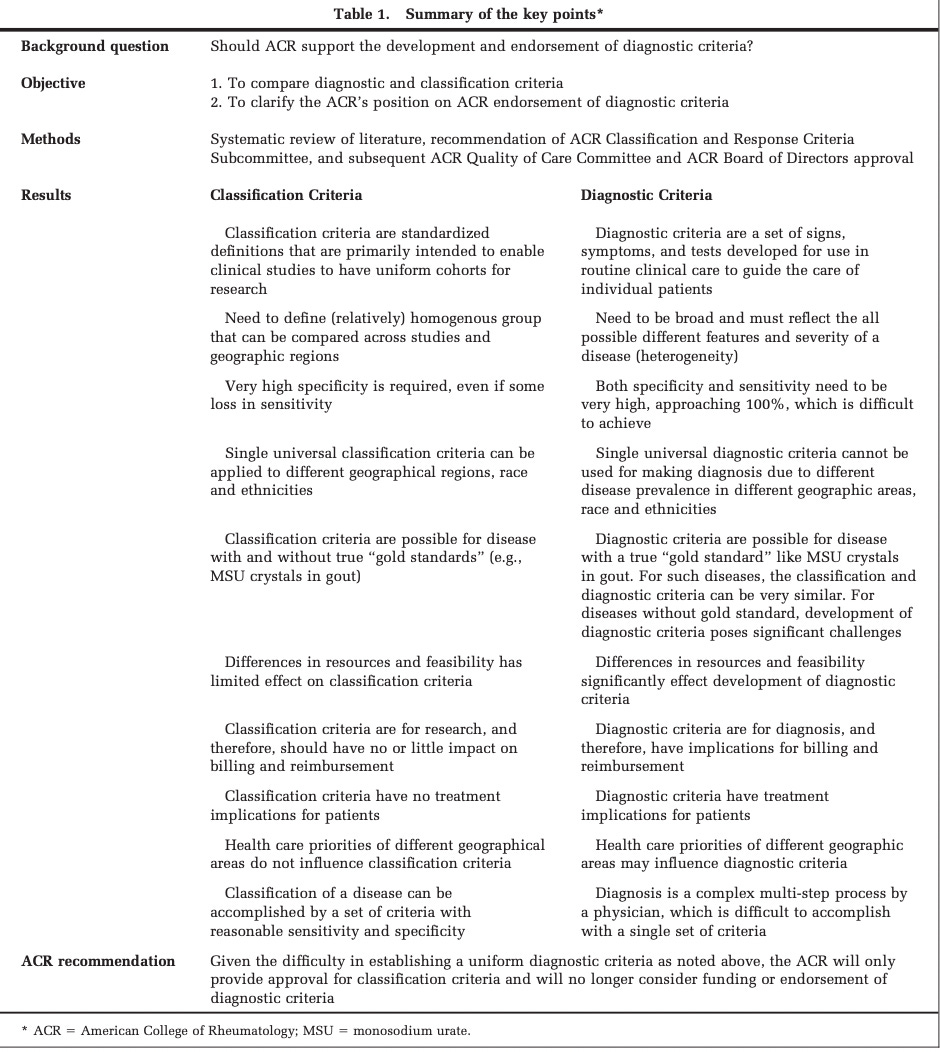
Distinctions Between Diagnostic and Classification Criteria? explains why the American College of Rheumatology will focus on defining classification criteria, but does not consider classification criteria to be diagnostic, and will no longer be defining diagnostic criteria for autoimmune rheumatological diseases. The table below sums up their position.
I Got Real Mad
The consequences of this decision for autoimmune disease sufferers are concerning. My initial reaction was that the American College of Rheumatology threw up its hands and said, boohoo, this is too hard. We’re going to abandon individual rheumatologists, and more importantly, their symptomatic patients, to staying constantly up-to-date on every research study, and critically evaluating each one on whether it should be incorporated into their individual practice. So that treatment and diagnostics will continue, indefinitely, to differ wildly from rheumatologist to rheumatologist, and from patient to patient. The research that is completed, based on our classification criteria, will have little practical relevance to the people who are actually diagnosed with the disease.
The article makes clear that what matters is that studies are consistent with themselves, as opposed to being broadly applicable. And here’s the direct quote to back that sentence up (emphasis in bold is mine).
Validated classification criteria are considered critical to the interpretation of study findings and comparisons of results between studies. Despite facilitating the comparison of study results, classification criteria have the potential to restrict the external validity of studies, because interventions may perform differently in study participants who fulfill classification criteria for a disease than in the broader group of patients in whom the same disease was diagnosed.
Most rheumatological conditions lack gold standard tests, so the American College of Rheumatology decided to halt development of diagnostic criteria and puts its faith in the clinical knowledge and judgement of individual rheumatologists as the “Gold Standard” of rheumatological diagnosis.
There are only a few validated diagnostic criteria in rheumatology, and clinicians commonly establish a diagnosis based on a subjective combination of clinical signs/symptoms, results of available clinical tests, and knowledge about epidemiology in their geographic area.
Needless to say, this long-standing, diagnostic “gold standard,” isn’t working well for people with autoimmune symptoms.
I Eventually Calmed Down
When I got over my anger a bit, I started to recognize that this was a public admission of how very little is really known about rheumatological autoimmune disease. The other limitations the American College of Rheumatology discuss is the geographic or financial availability of tests. They express concern about placing testing requirements on a diagnosis that could delay or prevent treatment. There’s also the issue of money. If diagnostic criteria is too stringent, and a patient doesn’t meet it, then insurance companies may refuse to cover healthcare for it. To be fair to the American College of Rheumatology’s position, they say that Classification Criteria and Diagnostic Criteria are on a spectrum that has the potential to converge once more research is completed and more is known about a given disease.
I’m concerned about how relevant diagnosis-based research on autoimmunity will be. The more I read, the more I see how important research into underlying genetics and immune system dysfunction is in autoimmunity, independent of a poorly-defined legacy of named autoimmune diseases. I don’t know if it’s possible to divorce the two in a research environment—looking out now for the study that does it.
References
Aggarwal, R., Ringold, S., Khanna, D., Neogi, T., Johnson, S.R., Miller, A., Brunner, H.I., Ogawa, R., Felson, D., Ogdie, A., Aletaha, D. and Feldman, B.M. (2015), Distinctions Between Diagnostic and Classification Criteria?. Arthritis Care & Research, 67: 891-897. https://doi.org/10.1002/acr.22583