So frequently, the disease process of autoimmunity is unmoored. There are few definitive things that are known, so diagnostic certainties are difficult to deliver. So, I feel a certain relief spending some time in the visualizable realm of the digestive tract. I wonder, is this degree of visual certainty one of the reasons gastroenterologists choose the specialty they do?
Compared to other body systems, the digestive tract is unique in that it’s actually considered to be external to the body. How can that be, when it seems so fundamentally internal? During the very early stages of human development, when cells are multiplying in three flat layers along the uterine wall, there is a point when that flat disc of cells, folds. This process is called “Embryonic folding.” This is the point at which humans become totally tubular, man (now, try forgetting that you’re fundamentally a food tube—and that’s my polite characterization). The inner part of that tube, which was originally external, becomes the digestive tract. The digestive tract communicates with the outside world by way of the mouth and the anus. Here’s a short video on the process of embryonic folding.
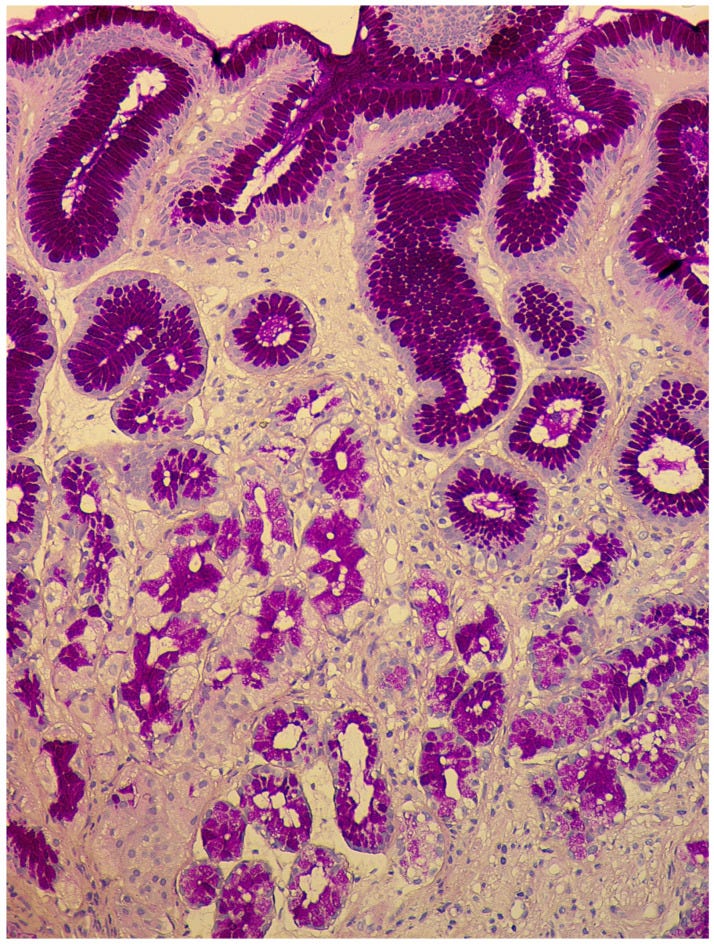
This concept has always totally blown my mind, and it makes sense that our digestive tract balances the functions of necessary-for-survival nutrient absorption and just-as-necessary-for-survival barrier and immune protection. As such, the digestive tract is susceptible to a myriad of external injuries and irritants, and then (over)active immune responses. Precisely because it is external to the body, the digestive tract is a port in the autoimmune storm, because you can see it. You can stick a camera in it and take a look at the tissue changes occurring most places along its length. You can take tissue samples and look at them under a microscope and characterize the features that you see, as they did in the above photo of late stage Autoimmune gastritis.
Because of it’s location in the stomach and ability to be seen, biopsied, and microscopically identified, Autoimmune gastritis has well-characterized diagnostic hallmarks that make finding study participants more straightforward. The authors of this 2016 Turkish study attempt to characterize age differences in the disease process of Autoimmune gastritis, with a particular emphasis on polyautoimmunity and Multiple autoimmune syndrome. Interestingly, unlike their 2017 study, which I reviewed in my last post, there was no confusion on the definition of polyautoimmunity and Multiple autoimmune syndrome in this study.
Area of Investigation
Multiple Autoimmune Syndrome: when one person meets the study classification criteria for three or more autoimmune diseases.
Study Title
Differences between older and young patients with autoimmune gastritis
Results
This study included 355 participants broken up into two groups: 119 participants who were 65 years of age, or older, and 236 participants who were younger than age 65. The differences between the older and younger groups were revealing, and suggest that clinicians need to be looking for different hallmarks of disease in younger vs. older patients. The results also suggest that older participants may have more damage to their stomachs than younger participants.
Older Participants
Older participants were more likely to have Vitamin B12 and iron deficiency as their presenting symptoms, not gastrointestinal symptoms. 84 of 119 older participants had B12 or iron deficiencies, compared to 35 participants with gastrointestinal symptoms.
Serum gastrin (“A hormone released from special cells in the lining of the stomach after eating.” NIH Cancer Institute) and chromogranin A levels (a non-specific marker that can indicate cell overgrowth) were significantly higher in older patients, representing greater stomach atrophy, and a higher degree of tissue damage, than younger participants. A significantly prolonged gastric emptying time was observed in older patients compared with younger patients. High serum gastrin and chromagranin levels were associated with an increased risk of delayed gastric emptying.
Serum vitamin B12 was lower in older patients as well. Pernicious anemia was more common in older participants than younger ones (present in 78 (65.5%) of participants). Enterochromograffin-like cell overgrowth was also more common in older patients.
Polyautoimmunity was more common in this group, and present in 79 (66.3%) participants. Multiple autoimmune syndrome was present in 21 (17.6%) participants. Autoimmune thyroiditis was the most common co-occurring autoimmune disease in participants of both age groups. Autoimmune thyroiditis and Rheumatoid arthritis were the most common autoimmune diseases in older participants with Multiple autoimmune syndrome.
Younger Participants
In the younger group, 200 participants were investigated for Autoimmune gastritis due to gastrointestinal symptoms, and 36 were investigated for Autoimmune gastritis due to Vitamin B12 or iron deficiency. Polyautoimmunity was less common in this group, and present in 58 (24.5%) participants. Multiple autoimmune syndrome was present in 13 (5.5%) participants. Pernicious anemia was less common with 29 (12.2%) participants with pernicious anemia. Anti-Hp immunoglobulin G and antiparietal cell antibodies were more commonly seen in younger patients, which could represent a more robust immune response generally seen in younger patients, or it could represent an earlier stage of the disease, prior to atrophic damage to the stomach.
Risk Factors for Polyautoimmunity
High serum gastrin and chromogranin A levels, as well as enterochromograffin-like cell overgrowth was associated with an increased risk of polyautoimmunity in study participants.
Why it Matters
Vitamin B12 and iron deficiency are relatively common conditions in patients who are 65 years of age and older. This study shows that there should be a high suspicion for Autoimmune causes of vitamin B12 and iron deficiency, even in the absence of gastrointestinal symptoms. Older patients with Autoimmune gastritis should be screened for Polyautoimmunity, particularly Autoimmune thyroid disease. Further studies are needed—always!—but this study hints at the need for early diagnosis and treatment to prevent atrophy of the stomach and the resultant nutrient absorption problems that atrophy creates. In this study, Polyautoimmunity is again more prevalent in older participants, pointing to a likely evolution over time, especially if left unidentified and thus untreated.
Study Type
For reference, I have ranked medical study types in order of least likely to be affected by hidden bias to most likely to be affected. Those studies that are most likely to be affected by hidden bias should be taken seriously, but not given the same weight as studies that are less likely to be affected by hidden bias. This study’s type appears in bold below.
Clinical Trial
Observational Study
Prospective
Retrospective
Cross-sectional
References
Kalkan Ç, Soykan I. Differences between older and young patients with autoimmune gastritis. Geriatr Gerontol Int. 2017 Jul;17(7):1090-1095. doi: 10.1111/ggi.12832. Epub 2016 Jul 22. PMID: 27444719.
Livzan MA, Gaus OV, Mozgovoi SI, Bordin DS. Chronic Autoimmune Gastritis: Modern Diagnostic Principles. Diagnostics (Basel). 2021 Nov 15;11(11):2113. doi: 10.3390/diagnostics11112113. PMID: 34829460; PMCID: PMC8621657.



