Summary
Juvenile idiopathic arthritis, formerly known as juvenile rheumatoid arthritis, is the most common type of arthritis in children under the age of 16.
Juvenile idiopathic arthritis can cause persistent joint pain, swelling and stiffness. Some children may experience symptoms for only a few months, while others have symptoms for many years.
Some types of juvenile idiopathic arthritis can cause serious complications, such as growth problems, joint damage and eye inflammation. Treatment focuses on controlling pain and inflammation, improving function, and preventing damage.
(Autoimmune Association, 2022)
Juvenile idiopathic arthritis
In JIA, autoantibodies target healthy joint cells and tissues. Formerly known as juvenile rheumatoid arthritis, JIA is a diagnosis that covers all forms of arthritis in individuals under 16 that last more than 6 weeks and whose origin is unknown.
JIA can arise in 6 different subtypes:
Oligoarthritis
Polyarthritis
Systemic-onset (Still’s Disease)
Enthesitis-related
Undifferentiated
Adult-Onset Still’s disease
When diagnosed in adults, JIA is more commonly called adult-onset Still’s disease. Some people only experience one episode of Still’s disease, but for others, it can cause chronic progressive illness.
The cause of Still’s disease is unknown, though several different treatments are available to help manage symptoms. As symptoms, progression, and severity differ widely amongst individuals with Still’s, the disease can be challenging to diagnose and treat.
(Global Autoimmune Institute, 2023)
Symptoms
The most common signs and symptoms of juvenile idiopathic arthritis are:
Pain. While your child might not complain of joint pain, you may notice that he or she limps — especially first thing in the morning or after a nap.
Swelling. Joint swelling is common but is often first noticed in larger joints such as the knee.
Stiffness. You might notice that your child appears clumsier than usual, particularly in the morning or after naps.
Fever, swollen lymph nodes and rash. In some cases, high fever, swollen lymph nodes or a rash on the trunk may occur — which is usually worse in the evenings.
Juvenile idiopathic arthritis can affect one joint or many. There are several different subtypes of juvenile idiopathic arthritis, but the main ones are systemic, oligoarticular and polyarticular. Which type your child has depends on symptoms, the number of joints affected, and if a fever and rashes are prominent features.
Like other forms of arthritis, juvenile idiopathic arthritis is characterized by times when symptoms flare up and times when symptoms may be minimal.
(Autoimmune Association, 2022)
Juvenile idiopathic arthritis
Joint pain, swelling, stiffness, fevers, swollen lymph nodes, and rashes (particularly on the torso of the body).
Adult-Onset Still’s disease
Joint pain, recurrent high fevers, skin rash, muscle pain, and sore throat.
(Global Autoimmune Institute, 2023)
Diagnostic Criteria
None. (Aggarwal et al, 2015)
Study Classification Criteria
Juvenile idiopathic arthritis (JIA)
An evidence-based classification criteria process was started in 2019 by the Pediatric Rheumatology International Trials Organization (Martini et. al, 2019). It is still in the process of being developed. The implication is that the following classification criteria, originally developed in 2001, then modified in 2004, by the International League of Associations for Rheumatology, is not evidence based. Nonetheless, it has been used as the basis for research over more than 20 years, and in the absence of other finalized criteria, is still being used today. It’s probable that the evidence-based criteria under development now by the Pediatric Rheumatology International Trials Organization would not be possible without the standardized research the 2001/2004 International League of Associations for Rheumatology criteria enabled.
General Definition of JIA
Juvenile idiopathic arthritis is arthritis of unknown etiology {cause} that begins before the 16th birthday and persists for at least 6 weeks; other known conditions are excluded.
Exclusions
The principle of this classification is that all categories of JIA are mutually exclusive. This principle is reflected in the list of possible exclusions for each category:
a. Psoriasis or a history of psoriasis in the patient or first-degree relative.
b. Arthritis in an HLA-B27 positive male beginning after the 6th birthday.
c. Ankylosing spondylitis, enthesitis related arthritis, sacroiliitis with inflammatory bowel disease, Reiter’s syndrome, or acute anterior uveitis, or a history of one of these disorders in a first-degree relative.
d. The presence of IgM rheumatoid factor on at least 2 occasions at least 3 months apart.
e. The presence of systemic JIA in the patient.
The application of exclusions is indicated under each category, and may change as new data become available.
Categories
Systemic Arthritis
Definition: Arthritis in one or more joints with or preceded by fever of at least 2 weeks’ duration that is documented to be daily (“quotidian”) for at least 3 days, and accompanied by one or more of the following:
Evanescent (nonfixed) erythematous rash
Generalized lymph node enlargement
Hepatomegaly and/or splenomegaly
Serositis
Exclusions: a, b, c, d.
Oligoarthritis
Definition: Arthritis affecting one to 4 joints during the first 6 months of disease. Two subcategories are recognized:
Persistent oligoarthritis: Affecting not more than 4 joints throughout the disease course
Extended oligoarthritis: Affecting a total of more than 4 joints after the first 6 months of disease
Exclusions: a, b, c, d, e.
Polyarthritis (Rheumatoid Factor {RF} Negative)
Definition: Arthritis affecting 5 or more joints during the first 6 months of disease; a test for RF is negative.
Exclusions: a, b, c, d, e.
Polyarthritis (Rheumatoid Factor Positive)
Definition: Arthritis affecting 5 or more joints during the first 6 months of disease; 2 or more tests for RF at least 3 months apart during the first 6 months of disease are positive.
Exclusions: a, b, c, e.
Psoriatic Arthritis
Definition: Arthritis and psoriasis, or arthritis and at least 2 of the following:
Dactylitis {Finger swelling}
Nail pitting or onycholysis {separation of the nail from the nail bed}
Psoriasis in a first-degree relative
Exclusions: b, c, d, e.
Enthesitis Related Arthritis
Definition: Arthritis and enthesitis, or arthritis or enthesitis with at least 2 of the following:
The presence of or a history of sacroiliac {joints that run parallel to the spine on either side} joint tenderness and/or inflammatory lumbosacral {low back} pain
The presence of HLA-B27 antigen
Onset of arthritis in a male over 6 years of age
Acute (symptomatic) anterior uveitis {inflammation of a front part of the eye}
History of ankylosing spondylitis, enthesitis related arthritis, sacroiliitis with inflammatory bowel disease, Reiter’s syndrome, or acute anterior uveitis in a first-degree relative
Exclusions: a, d, e.
Undifferentiated Arthritis
Definition: Arthritis that fulfills criteria in no category or in 2 or more of the above categories.
Descriptors
A number of “descriptors” have been proposed to gather further information on the patterns of the clinical picture. These include age at onset, further description of the arthritis (large joints, small joints, symmetry, upper or lower limb predominance, and individual joint involvement), disease course (number of joints), presence of ANA {antinuclear antibodies}, chronic or acute anterior uveitis, and the HLA allelic associations. The potential value of ANA as a diagnostic criterion has received a great deal of attention, but there is insufficient evidence to support its inclusion at this time. The descriptors are not part of the classification of JIA, but new data about them may allow reclassification in the future.
Definitions of Terms
Arthritis: Swelling within a joint, or limitation in the range of joint movement with joint pain or tenderness, which persists for at least 6 weeks, is observed by a physician, and is not due to primarily mechanical disorders or to other identifiable causes.
Dactylitis: Swelling of one or more digits, usually in an asymmetric distribution, which extends beyond the joint margin.
Enthesitis: Tenderness at the insertion of a tendon, ligament, joint capsule, or fascia to bone.
Inflammatory lumbosacral pain: Lumbosacral spinal pain at rest with morning stiffness that improves on movement.
Nail pitting: A minimum of 2 pits on one or more nails at any time.
Number of affected joints: Joints that can be individually evaluated clinically are counted as separate joints.
Positive test for rheumatoid factor (RF): At least 2 positive results (as routinely defined in an accredited laboratory), at least 3 months apart, during the first 6 months of disease.
Psoriasis: As diagnosed by a physician (but not necessarily a dermatologist).
Quotidian fever: Fever that rises to ≥ 39°C once a day and returns to ≤ 37°C between fever peaks.
Serositis: Pericarditis and/or pleuritis and/or peritonitis.
Sacroiliac joint arthritis: Presence of tenderness on direct compression over the sacroiliac joints.
Spondyloarthropathy: Inflammation of entheses and joints of the lumbosacral spine.
Uveitis: Chronic anterior uveitis as diagnosed by an ophthalmologist.
(Petty et. al, 2004)
2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis
Macrophage activation syndrome (MAS) is the term used to describe a potentially life-threatening complication of systemic inflammatory disorders, which occurs most commonly in systemic juvenile idiopathic arthritis (JIA) and in its adult equivalent, adult-onset Still’s disease (1–4), although its occurrence in patients with other autoimmune or autoinflammatory conditions, i.e., adult- and childhood-onset systemic lupus erythematosus (5,6), Kawasaki disease (7,8), and periodic fever syndromes (9,10), is being reported with increased frequency. MAS is characterized by an overwhelming inflammatory reaction due to an uncontrolled and dysfunctional immune response involving the continual activation and expansion of T lymphocytes and macrophages, which results in massive hypersecretion of proinflammatory cytokines (11,12).
(Ravelli et. al, 2016)
Pediatric Rheumatology International Trials Organization Preliminary 2019 Classification Criteria
(Zaripova et. al, 2021)
Adult-onset Still’s disease
(Korty et. al, 2019)
The sensitivity and specificity of both of the above criteria for Adult-onset Still’s disease were studied by Lebrun et. al here.
The table below provides a super-helpful side-by-side comparison of the Yamaguchi and Fautrel criteria for Adult-onset Still’s disease, AND the current criteria for systemic Juvenile idiopathic arthritis:
(Tomaras et. al, 2021)
Criteria differences lead to delays in pediatric diagnosis: “As the paediatric criteria require the presence of an arthritis a subset of SoJIA patients can have a severe delay in diagnosis as the systemic symptoms can proceed the arthritis by up to 10 years [135]. Retrospective testing of the Yamaguchi criteria in paediatric patients with suspected SoJIA with and without arthritis has yielded promising results especially for SoJIA patients with a delay in onset of arthritis [136]. Combining both sets of criteria might improve the time until diagnosis, especially in patients with a long time between systemic onset and beginning of arthritis [137]. A treatment window targeting the cytokine driven first phase of the disease might otherwise close [138].” (Tomaras et. al, 2021)
Diagnostic Tests
Juvenile idiopathic arthritis
Ultrasound and MRI (Sudoł-Szopińska et. al, 2016)
Rheumatoid Factor blood test to differentiate between sub-types, where other clinical features are present
Adult-onset Still’s disease
Complete blood count (CBC) with differential to specifically measure abnormally high levels of a type of white blood cell called a neutrophil, and abnormally high levels of all the white blood cells added together. (Narváez Garcia et. al, 2017)
Indicates a general autoimmune process in the absence of infectious disease. Non-specific to Adult-onset Still’s disease.
Increased blood levels of ferritin (the storage form of iron). (Narváez Garcia et. al, 2017)
More specific to this disease when taken in the context of other symptoms, but results can be elevated in other non-autoimmune conditions
“In addition, 96% of patients with atypical cutaneous manifestations presented hyperferritinemia {increased blood levels of ferritin}. During AOSD, persistent high serum levels of ferritin may be observed; it is an iron storage protein composed of 24 subunits, heavy (H) subunits and light (L) subunits. The ferritin enriched in L subunits (L-ferritin) and the ferritin enriched in H subunits (H-ferritin) may be observed in different tissues.[49] Recently, Ruscitti et al[49] have demonstrated an increased skin expression of H-ferritin in the biopsies obtained from persistent cutaneous lesions of AOSD patients, associated with a strong infiltrate of CD68+/H-ferritin+ cells. This finding seems to have clinical implications as according to their findings there is a correlation between both, the tissue H-ferritin levels and the CD68+/H-ferritin+ cells, with the severity of the clinical picture and the multi-visceral {organ} involvement of the disease.” (Narváez Garcia et. al, 2017)
“Moreover, ferritin is a very helpful serologic marker for diagnosis and follow-up, especially when it increases >5-fold. Current propositions for hyperferritinaemia in AoSD include increased production by macrophages, liver and erythrocytes due to parallel erythrophagocytosis [46,47,48,49]. Furthermore, high circulating ferritin has a positive feedback mechanism that can further exacerbate its own inflammatory properties [24]. Ferritin contains two types of subunits: heavy (H) and light (L). In the bone marrow of patients with MAS {macrophage activation syndrome}, high levels of H-ferritin are found, and they correlate with disease severity. Correspondingly, lymph nodes and skin are infiltrated with CD68/H-ferritin cells.” (Tomaras et. al, 2021)
Rash biopsy
In cases of hives/hives-like rashes and widespread, non-itching, persistent skin redness, “biopsy specimens reveal a nonspecific slight to moderate inflammatory infiltrate in the upper dermis, similar to that observed in biopsies of the typical evanescent skin rash.[1–3,43] Thus, a skin biopsy of atypical eruptions is recommended (specially in patients who do not yet fulfill the Yamaguchi criteria) because the…” tissue features “…can be considered to be highly suggestive of” Adult-onset Still’s disease. (Narváez Garcia et. al, 2017)
Organized Autoimmunity
(Alternative Autoimmune Disease Classification: FIEM, MIEM or BIEM, or FEM, MEM or BEM)
sex predominance (is an autoimmune disease primarily found in genetic Females, Males, or equally in Both?)
Juvenile idiopathic arthritis
Oligoarthritis: Female predominance
Polyarthritis (Rheumatoid Factor Negative): Female predominance
Polyarthritis (Rheumatoid Factor Positive): Female predominance
Systemic: Both
Enthesitis Related: Male predominance
Psoriatic: Two sources list different predominance 1. Female predominance (Kim et. al, 2017) and 2. Both (Zaripova et. al, 2021)
Adult-onset Still’s disease
A couple of studies with small sample sizes show an approximate Female predominance of 60-70% (Lenert et. al, 2020) (Nossent et. al, 2022). More data is needed for a clearer picture of sex predominance.
Inherited and acquired gene variations that cause increased susceptibility
Human Leukocyte Antigen (HLA) Associations
Juvenile idiopathic arthritis, subtype Enthesitis-related arthritis: HLA B27 (45-85% of patients studied), DRB1*01, DQA1*01, DQB1*05 (Zaripova et. al, 2021).
Juvenile idiopathic arthritis, subtype Psoriatic:
(HLA)-DR5 (Brunello et. al, 2022).
HLA DRB1*01, DRB1*11, DRB1*12, HLA-C*06 - biomarker for skin involvement, HLA B27 – for sacroiliitis (mostly in older age) (Zaripova et. al, 2021).
Juvenile idiopathic arthritis, subtype Oligoarticular: HLA A2, DRB1*11, DRB1*08, DPB1*0201, DRB1*15*01, DQA1*04, DQB1*04, DRB1*13 for persistent, DRB1*01 for extended variant (Zaripova et. al, 2021).
Juvenile idiopathic arthritis, subtype Polyarticular Rheumatoid Factor Negative: HLA A2, DRB1*08, DPB1:03, DQA1*04, DRB1*15*01, DPB1*02*01 (Zaripova et. al, 2021).
Juvenile idiopathic arthritis, subtype Polyarticular Rheumatoid Factor Positive: HLA DRB1*04, DRB1*01, DRB1*08, DQA1*03 (Zaripova et. al, 2021).
Juvenile idiopathic arthritis, subtype systemic: HLA DRB1:04, DQA1*01, DQB1*04, DRB1*01 (Zaripova et. al, 2021).
“Several studies have documented genetic associations to JIA [21–25]. Genetic linkage depends on subtype and may be divided into two groups: HLA genes and non-HLA-related genes. Meta-analysis of genetic predisposition to JIA subtypes has shown association with HLA class II molecules (A2, DRB1, DPB1) mostly for non-systemic subtypes (Table (Table1),1), while for sJIA the lack of association with HLA genes has been found [21].” (Zaripova et. al, 2021)
Other Gene Variations (mutations)
Juvenile idiopathic arthritis, subtype systemic “More recently a locus on chromosome 1 and loci within the HLA class II and III region on chromosome 6 have been associated with SoJIA [113]. Furthermore, HLA-DRB1*11 was found to be a major risk factor for SoJIA indicating the involvement of antigen-specific T cells [114]”(Tomaras et. al, 2021).
LACC1. There is “emerging evidence” that variations on this single gene cause a rare form of systemic Juvenile idiopathic arthritis that runs in families (Tomaras et. al, 2021).
Gene Triggering Environmental Exposures
Adult-onset Still’s disease
Infections
cytomegalovirus (Tomaras et. al, 2021)
Epstein-Barr virus (Tomaras et. al, 2021)
influenza (Tomaras et. al, 2021)
Mycoplasma (Tomaras et. al, 2021)
hepatitis (Tomaras et. al, 2021)
Toxins
Unknown
Stress
Needs to be assessed for each patient
Multiple interactive and destructive immune system pathologies
Systemic Juvenile idiopathic arthritis and Adult-onset Still’s disease
Innate (immediate) immune response
Interleukin-1 Beta
Interleukin-18 (a pro-inflammatory cytokine, which is a protein that exerts an effect on the immune system, and whose action is counteracted by interleukin-18 binding protein) (Girard-Guyonvarc, 2022)
Interleukin-6 (Nirmala et. al, 2015)
S100 Proteins (Nirmala et. al, 2015)
Neutrophils (Kim JW et. al, 2021)
Adult-onset Still’s disease
Innate (immediate) immune response
Interleukin-1 Beta and Interleukin-18 (pro-inflammatory cytokines, or proteins that have an effect on the immune system) are overproduced, which causes
“cytokine bursts” of Interleukin-6, Interleukin-8, Interleukin-17, Interleukin-18 and Tumor Necrosis Factor-alpha (Tomaras et. al, 2021)
anti-inflammatory cytokine Interleukin-10 (Sun et. al, 2019)
{Why would an anti-inflammatory cytokine contribute to the disease process?} Check this reference for more information: Ip WKE, Hoshi N, Shouval DS, Snapper S, Medzhitov R. Anti-inflammatory effect of IL-10 mediated by metabolic reprogramming of macrophages. Science. 2017;356(6337):513–519. doi: 10.1126/science.aal3535. [PMC free article][PubMed] [CrossRef] [Google Scholar] [Ref list]
Psoriatic Juvenile idiopathic arthritis
Anti-nuclear antibodies in younger children around 2 years of age (Brunello et. al, 2022)
Anti-nuclear antibodies in 50% of patients studied (Zaripova et. al, 2021)
Oligoarticular juvenile idiopathic arthritis
Anti-nuclear antibodies in 60% of patients studied (Zaripova et. al, 2021)
Polyarticular juvenile idiopathic arthritis
Rheumatoid Factor negative-type
Anti-nuclear antibodies in 40% of patients studied (Zaripova et. al, 2021)
Rheumatoid Factor positive-type
Rheumatoid factor (Zaripova et. al, 2021)
Anti-citric citrullinated peptide (Zaripova et. al, 2021)
Anti-nuclear antibodies in 40% of patients studied (Zaripova et. al, 2021)
Tissue-Type or Cell-Type Attacked
Juvenile idiopathic arthritis
This useful side-by-side comparison illustrates the joint damage that can—although doesn’t always—occur with all forms of Juvenile idiopathic arthritis:
(Zaripova et. al, 2021)
Oligoarthritis
See image above
Polyarthritis
Rheumatoid factor negative
See image above
Rheumatoid factor positive
See image above
Psoriatic
See image above
Skin tissue/cell-type damaged
Under investigation
Enthesitis-related
See image above
{What differentiates enthesitis-specific arthritis from the generalized joint damage pictured above?}
Undifferentiated
See image above
systemic Juvenile idiopathic arthritis and Adult-onset Still’s disease
Lungs
Spleen
Liver
Fluid-filled spaces around vital organs (serositis)
joints (see above image)
Treatment(s)
Juvenile idiopathic arthritis (non-systemic polyarthritis (5 or more joints are affected), sacroiliitis (inflammation of the rear end hip joints that run parallel to the spine), or enthesitis types (inflammation of where tendons and/or ligaments insert into bone))
Non-steroidal anti-inflammatory drugs (Ringold et. al, 2019)
Systemic glucocorticoids (Ringold et. al, 2019)
Intraarticular glucocorticoids
Triamcinolone Acetonide
Triamcinolone Hexacetonide
Methylprednisolone Acetate
(Ringold et. al, 2019)
Non-biologic disease modifying antirheumatic drugs
Leflunomide
Methotrexate
Sulfasalazine
Triple non-biologic disease modifying anti rheumatic drugs (methotrexate, sulfasalazine, hydroxychloroquine)
(Ringold et. al, 2019)
Biologic disease modifying antirheumatic drugs
Tumor necrosis factor alpha inhibitors (TNFi)
Adalimumab
Etanercept
Infliximab
Golimumab
Non-TNFi Biologics
Abatacept (CTLA4-Ig)
Tocilizumab (anti-Interleukin-6R)
Rituximab (anti-CD20)
(Ringold et. al, 2019)
This helpful algorithmic pictogram shows the American College of Rheumatology’s broad guidelines, which they make clear here, are intended to be as flexible and non-restrictive as possible, since the level of scientific evidence to support these guidelines is low.
(Ringold et. al, 2019)
Systemic Juvenile idiopathic arthritis
Interleukin-1 inhibitors
Anakinra. “Anakinra is licensed for subcutaneous use for systemic juvenile idiopathic arthritis, periodic fever syndromes, rheumatoid arthritis and AoSD (only by the European Medicines Agency)” (Tomaras et. al, 2021).
Canakinumab, defined as “a high-affinity human monoclonal anti − IL-1β antibody”(Nirmala et. al, 2015). “Canakinumab is currently licensed for AoSD, SoJIA, periodic fever syndromes and gout” (Tomaras et. al, 2021).
Rilanocept. “The efficacy and safety of another IL-inhibitor, rilonacept, was analyzed in a randomized, double-blind, placebo-controlled trial with seventy-one children with SoJIA. Rilonacept showed some benefit with an acceptable safety profile, although the primary end point was not met [100]” (Tomaras et. al, 2021).
Interleukin-18 binding protein, preliminary data only (Girard-Guyonvarc, 2022)
“Tadekinig alpha, a recombinant human IL-18 binding protein, demonstrated its potential effectiveness and acceptable safety profile in a phase 2 multicentred European study in 2018. The low number of participants (21) and the short period of treatment duration (12 weeks) could be considered limiting factors [110]” (Tomaras et. al, 2021).
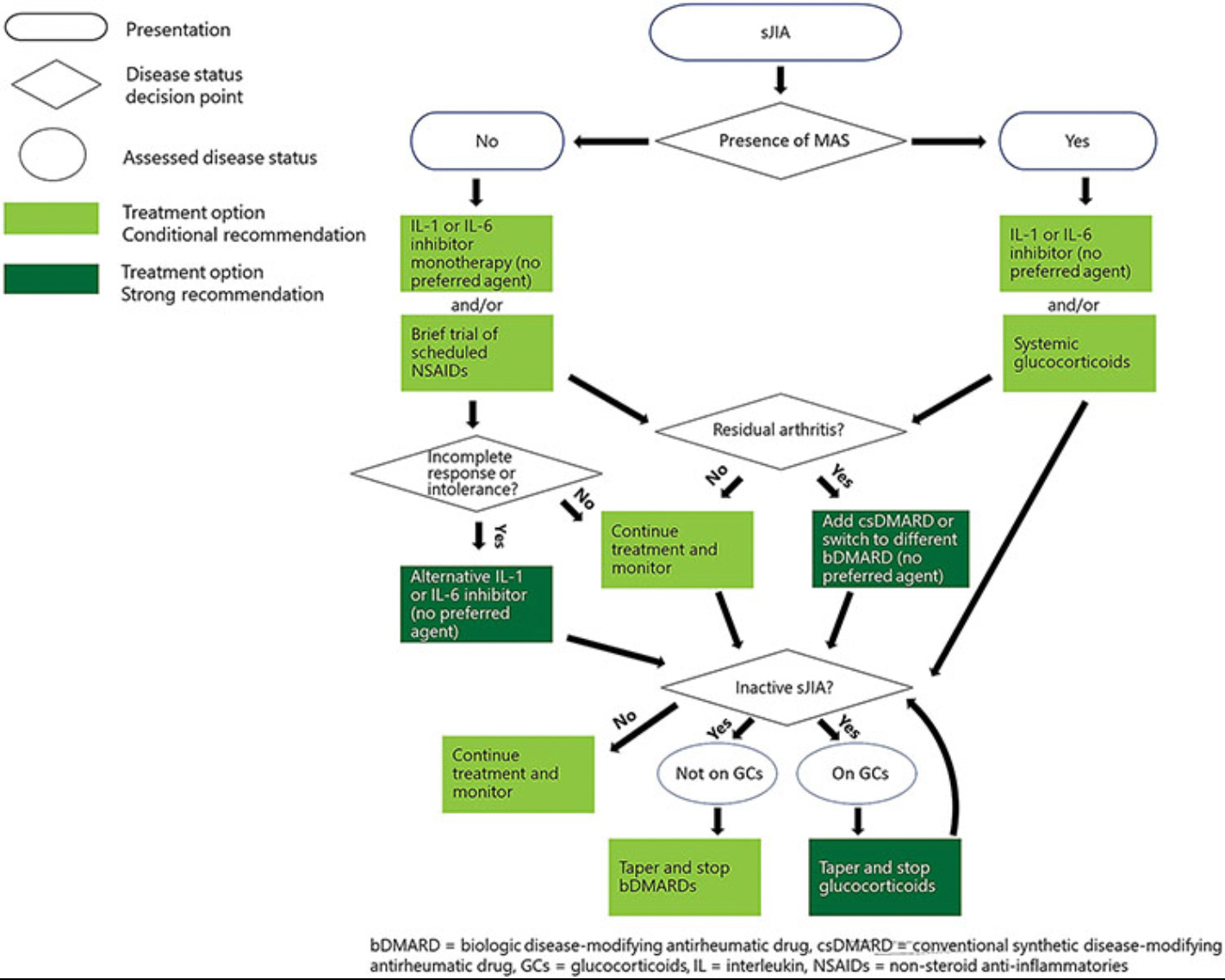
The American College of Rheumatology provides this treatment algorithm:
(Onel et al, 2022)
Adult-onset Still’s disease
Interleukin-1 inhibitors
Anakinra. “Anakinra, a recombinant humanized IL-1 receptor antagonist, is the first choice for AoSD, yet patients with mainly articular phenotypes do not always benefit” (Tomaras et. al, 2021).
Canakinumab, defined as “a high-affinity human monoclonal anti − IL-1β antibody”(Nirmala et. al, 2015). “Canakinumab is currently licensed for AoSD, SoJIA, periodic fever syndromes and gout” (Tomaras et. al, 2021).
Interleukin-6 inhibitors
Tocilizumab. “Tocilizumab, a humanized monoclonal antibody against the IL-6 receptor, showed promising results in the treatment of AoSD in a pilot study. Both the systemic features and the arthritic manifestations improved [101,102,103]. A 2018 meta-analysis investigated the benefits of tocilizumab in patients with AoSD and definitely showed signals of efficacy compared to conventional therapy regimes and was well acceptable in terms of safety [104]” (Tomaras et. al, 2021).
Sarilumab. “The other IL-6 receptor antagonist, sarilumab, was reported to be effective as a steroid-sparing agent [105]” (Tomaras et. al, 2021).
Interleukin-18 binding protein, preliminary data only (Girard-Guyonvarc, 2022)
Janus kinase inhibitors “block a wide variety of proinflammatory cells” (Tomaras et. al, 2021).
tofacitinib, preliminary data only
Baricitinib, preliminary and conflicting data
This is a helpful suggested treatment algorithm:
(Tomaras et. al, 2021)
Oligoarthritis
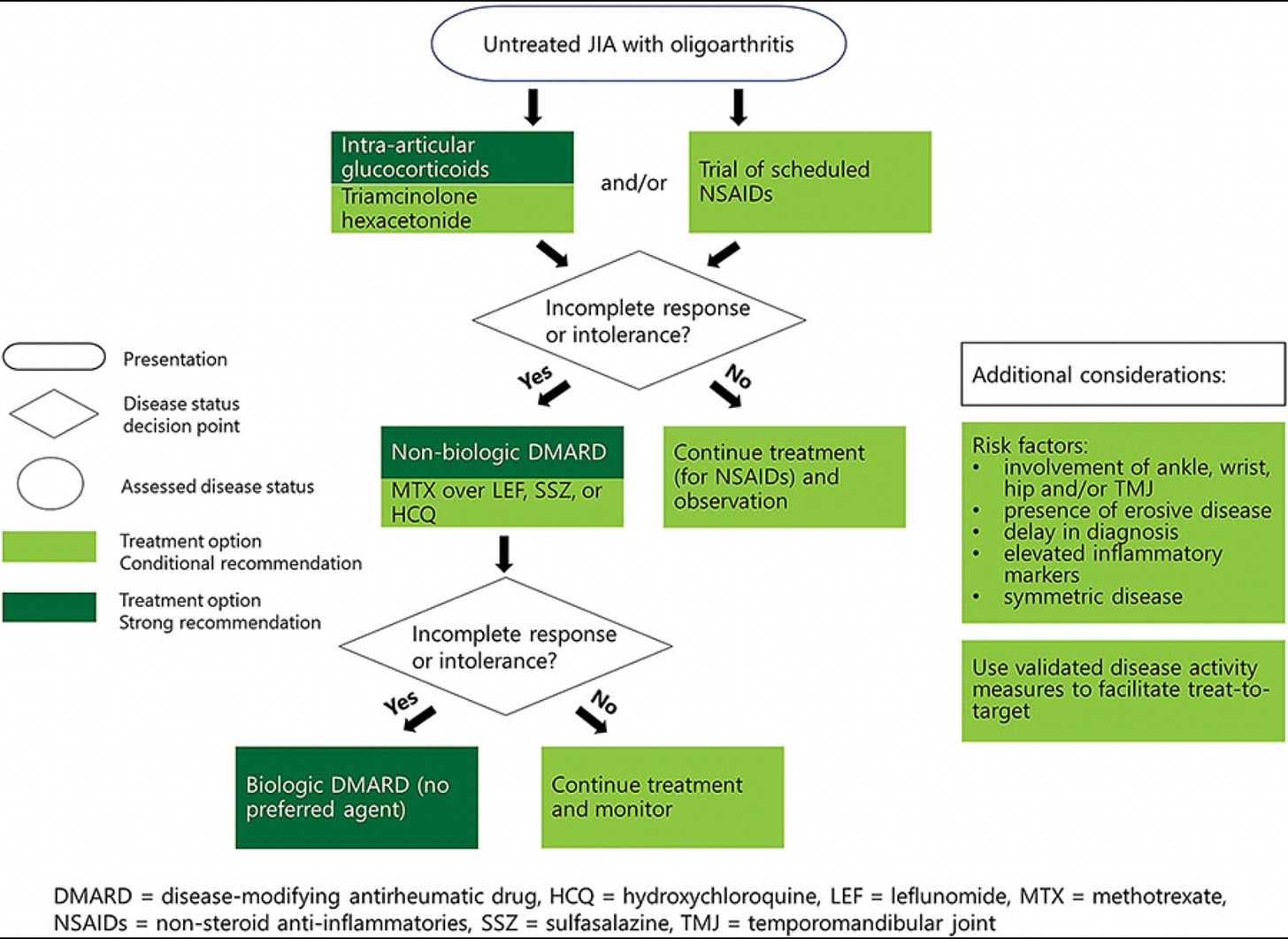
A treatment algorithm from the American College of Rheumatology:
(Onel et al, 2022)
Temperomandibular joint arthritis
A treatment algorithm from the American College of Rheumatology:
(Onel et al, 2022)
Managing Specialist(s)
Rheumatologist
Ophthalmologist
Dermatologist
Research Authors
Too numerous to list comprehensively.
Research Institutions
Too numerous to list comprehensively.
Average Time from Symptom Onset to Diagnosis
Adult-onset Still’s disease
1.5-4 years (Tomaras et. al, 2021).
Juvenile idiopathic arthritis
Unclear. Likely to be type-dependent.
Last Updated
May 15, 2023
References
Aggarwal, R., Ringold, S., Khanna, D., Neogi, T., Johnson, S.R., Miller, A., Brunner, H.I., Ogawa, R., Felson, D., Ogdie, A., Aletaha, D. and Feldman, B.M. (2015), Distinctions Between Diagnostic and Classification Criteria?. Arthritis Care & Research, 67: 891-897. https://doi.org/10.1002/acr.22583
Brunello F, Tirelli F, Pegoraro L, Dell'Apa F, Alfisi A, Calzamatta G, Folisi C, Zulian F. New Insights on Juvenile Psoriatic Arthritis. Front Pediatr. 2022 May 26;10:884727. doi: 10.3389/fped.2022.884727. PMID: 35722498; PMCID: PMC9199423.
Girard-Guyonvarc'h C, Harel M, Gabay C. The Role of Interleukin 18/Interleukin 18-Binding Protein in Adult-Onset Still's Disease and Systemic Juvenile Idiopathic Arthritis. J Clin Med. 2022 Jan 15;11(2):430. doi: 10.3390/jcm11020430. PMID: 35054124; PMCID: PMC8781628.
Juvenile arthritis. Autoimmune Association. (2022, November 10). Retrieved April 17, 2023 from https://autoimmune.org/disease-information/juvenile-arthritis/
JUVENILE IDIOPATHIC ARTHRITIS (JIA)/ADULT-ONSET STILL'S DISEASE. Global Autoimmune Institute. (2023). Retrieved April 17, 2023 from https://www.autoimmuneinstitute.org/juvenile-idiopathic-arthritis-stills/
Kim JW, Ahn MH, Jung JY, Suh CH, Kim HA. An Update on the Pathogenic Role of Neutrophils in Systemic Juvenile Idiopathic Arthritis and Adult-Onset Still's Disease. Int J Mol Sci. 2021 Dec 2;22(23):13038. doi: 10.3390/ijms222313038. PMID: 34884842; PMCID: PMC8657670.
Kim YD, Job AV, Cho W. Differential Diagnosis of Juvenile Idiopathic Arthritis. J Rheum Dis 2017;24:131-137. https://doi.org/10.4078/jrd.2017.24.3.131
Korty T, Baxa K, Sahni K, Grunbaum A, Soto-Aguilar M. Case Report: An Adult-Onset Still’s Disease Mimic. The Rheumatologist. 2019 July. https://www.the-rheumatologist.org/article/case-report-an-adult-onset-stills-disease-mimic/?singlepage=1
Lebrun D, Mestrallet S, Dehoux M, Golmard JL, Granger B, Georgin-Lavialle S, Arnaud L, Grateau G, Pouchot J, Fautrel B. Validation of the Fautrel classification criteria for adult-onset Still's disease. Semin Arthritis Rheum. 2018 Feb;47(4):578-585. doi: 10.1016/j.semarthrit.2017.07.005. Epub 2017 Jul 12. PMID: 28760536.
Lenert A, Oh G, Ombrello MJ, Kim S. Clinical characteristics and comorbidities in adult-onset Still's disease using a large US administrative claims database. Rheumatology (Oxford). 2020 Jul 1;59(7):1725-1733. doi: 10.1093/rheumatology/kez622. PMID: 31965185; PMCID: PMC7310096.
Martini A, Ravelli A, Avcin T, Beresford MW, Burgos-Vargas R, Cuttica R, Ilowite NT, Khubchandani R, Laxer RM, Lovell DJ, Petty RE, Wallace CA, Wulffraat NM, Pistorio A, Ruperto N; Pediatric Rheumatology International Trials Organization (PRINTO). Toward New Classification Criteria for Juvenile Idiopathic Arthritis: First Steps, Pediatric Rheumatology International Trials Organization International Consensus. J Rheumatol. 2019 Feb;46(2):190-197. doi: 10.3899/jrheum.180168. Epub 2018 Oct 1. PMID: 30275259.
Narváez Garcia FJ, Pascual M, López de Recalde M, Juarez P, Morales-Ivorra I, Notario J, Jucglà A, Nolla JM. Adult-onset Still's disease with atypical cutaneous manifestations. Medicine (Baltimore). 2017 Mar;96(11):e6318. doi: 10.1097/MD.0000000000006318. PMID: 28296747; PMCID: PMC5369902.
Nirmala N, Brachat A, Feist E, Blank N, Specker C, Witt M, Zernicke J, Martini A, Junge G. Gene-expression analysis of adult-onset Still's disease and systemic juvenile idiopathic arthritis is consistent with a continuum of a single disease entity. Pediatr Rheumatol Online J. 2015 Nov 20;13:50. doi: 10.1186/s12969-015-0047-3. PMID: 26589963; PMCID: PMC4654831.
Nossent J, Raymond W, Keen H, Preen DB, Inderjeeth CA. Adult-onset Still's disease in Western Australia: Epidemiology, comorbidity and long-term outcome. Int J Rheum Dis. 2022 Nov;25(11):1306-1314. doi: 10.1111/1756-185X.14424. Epub 2022 Aug 24. PMID: 36004429; PMCID: PMC9805040.
Onel KB, Horton DB, Lovell DJ, Shenoi S, Cuello CA, Angeles-Han ST, Becker ML, Cron RQ, Feldman BM, Ferguson PJ, Gewanter H, Guzman J, Kimura Y, Lee T, Murphy K, Nigrovic PA, Ombrello MJ, Rabinovich CE, Tesher M, Twilt M, Klein-Gitelman M, Barbar-Smiley F, Cooper AM, Edelheit B, Gillispie-Taylor M, Hays K, Mannion ML, Peterson R, Flanagan E, Saad N, Sullivan N, Szymanski AM, Trachtman R, Turgunbaev M, Veiga K, Turner AS, Reston JT. 2021 American College of Rheumatology Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Oligoarthritis, Temporomandibular Joint Arthritis, and Systemic Juvenile Idiopathic Arthritis. Arthritis Care Res (Hoboken). 2022 Apr;74(4):521-537. doi: 10.1002/acr.24853. Epub 2022 Mar 1. PMID: 35233986; PMCID: PMC10124899.
Petty RE, Southwood TR, Manners P, Baum J, Glass DN, Goldenberg J, He X, Maldonado-Cocco J, Orozco-Alcala J, Prieur AM, Suarez-Almazor ME, Woo P; International League of Associations for Rheumatology. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004 Feb;31(2):390-2. PMID: 14760812.
Ravelli A, Minoia F, Davì S, Horne A, Bovis F, Pistorio A, Aricò M, Avcin T, Behrens EM, De Benedetti F, Filipovic L, Grom AA, Henter JI, Ilowite NT, Jordan MB, Khubchandani R, Kitoh T, Lehmberg K, Lovell DJ, Miettunen P, Nichols KE, Ozen S, Pachlopnik Schmid J, Ramanan AV, Russo R, Schneider R, Sterba G, Uziel Y, Wallace C, Wouters C, Wulffraat N, Demirkaya E, Brunner HI, Martini A, Ruperto N, Cron RQ; Paediatric Rheumatology International Trials Organisation; Childhood Arthritis and Rheumatology Research Alliance; Pediatric Rheumatology Collaborative Study Group; Histiocyte Society. 2016 Classification Criteria for Macrophage Activation Syndrome Complicating Systemic Juvenile Idiopathic Arthritis: A European League Against Rheumatism/American College of Rheumatology/Paediatric Rheumatology International Trials Organisation Collaborative Initiative. Arthritis Rheumatol. 2016 Mar;68(3):566-76. doi: 10.1002/art.39332. Epub 2016 Feb 9. PMID: 26314788.
Ringold S, Angeles-Han ST, Beukelman T, Lovell D, Cuello CA, Becker ML, Colbert RA, Feldman BM, Ferguson PJ, Gewanter H, Guzman J, Horonjeff J, Nigrovic PA, Ombrello MJ, Passo MH, Stoll ML, Rabinovich CE, Schneider R, Halyabar O, Hays K, Shah AA, Sullivan N, Szymanski AM, Turgunbaev M, Turner A, Reston J. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non-Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis Care Res (Hoboken). 2019 Jun;71(6):717-734. doi: 10.1002/acr.23870. Epub 2019 Apr 25. PMID: 31021516; PMCID: PMC6561125.
Sudoł-Szopińska I, Grochowska E, Gietka P, Płaza M, Pracoń G, Saied F, Walentowska-Janowicz M. Imaging of juvenile idiopathic arthritis. Part II: Ultrasonography and MRI. J Ultrason. 2016 Sep;16(66):237-51. doi: 10.15557/JoU.2016.0024. Epub 2016 Sep 7. PMID: 27679727; PMCID: PMC5034018.
Sun Y., Wang Z., Chi H., Hu Q., Ye J., Liu H., Cheng X., Shi H., Zhou Z., Teng J., et al. Elevated serum levels of interleukin-10 in adult-onset Still’s disease are associated with disease activity. Clin. Rheumatol. 2019;38:3205–3210. doi: 10.1007/s10067-019-04642-x.
Tomaras S, Goetzke CC, Kallinich T, Feist E. Adult-Onset Still's Disease: Clinical Aspects and Therapeutic Approach. J Clin Med. 2021 Feb 12;10(4):733. doi: 10.3390/jcm10040733. PMID: 33673234; PMCID: PMC7918550.
Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, Kashiwagi H, Kashiwazaki S, Tanimoto K, Matsumoto Y, Ota T, et al. Preliminary criteria for classification of adult Still's disease. J Rheumatol. 1992 Mar;19(3):424-30. PMID: 1578458.
Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. doi: 10.1186/s12969-021-00629-8. PMID: 34425842; PMCID: PMC8383464.