Summary
Polymyalgia rheumatica is characterized by muscle pain and stiffness in the neck, shoulder, and hip area. This stiffness, lasting about 30 minutes, is more severe upon waking or after a period of inactivity. Persons also may have “flu-like” symptoms. The symptoms may come on suddenly or gradually and usually strikes people over 50 years of age with age 70 the most common age of onset. There may be remission in one to several years. Up to 15% of persons develop giant cell arteritis (also called temporal arteritis), during or after polymyalgia symptoms appear.
(Autoimmune Association, 2023)
Characterized by muscle pain and stiffness in the neck, shoulders, and hips, equally affecting both sides of the body. The pain and discomfort are normally so great that it interferes with normal day-to-day activities. PR may appear overnight, or more gradually, and may last up to several years.
(Global Autoimmune Institute, 2023)
Symptoms
The signs and symptoms of polymyalgia rheumatica usually occur on both sides of the body and might include:
Aches or pain in your shoulders
Aches or pain in your neck, upper arms, buttocks, hips or thighs
Stiffness in affected areas, particularly in the morning or after being inactive for a time
Limited range of motion in affected areas
Pain or stiffness in your wrists, elbows or knees
You might also have more-general signs and symptoms, including:
Mild fever
Fatigue
A general feeling of not being well (malaise)
Loss of appetite
Unintended weight loss
Depression
(Autoimmune Association, 2023)
Stiffness after resting, aches and pains in the shoulders, neck, upper arms, buttock, hips or thighs, as well as limited range of motion in the areas that are affected, pain and stiffness in wrists, elbows, or knees, fever, weakness, weight loss, fatigue, malaise, loss of appetite and depression.
(Global Autoimmune Institute, 2023)
Diagnostic Criteria
It is not clear whether the Bird, Jones and Hazleman, Chuang and Hunder, and Healey criteria is intended to be diagnostic and/or classification criteria. The American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) criteria is intended as research study classification criteria only. The American College of Rheumatology stresses that classification criteria may be used to assist with diagnosis, but is used for different purposes and is not synonymous with diagnostic criteria.
(Fors et. al, 2019)
Study Classification Criteria
(Dasgupta et. al, 2012)
Diagnostic Tests
Abnormally elevated Estimated sedimentation rate (ESR)
Abnormally elevated C-reactive protein (CRP)
Rheumatoid factor (negative)
Antinuclear antibody (negative)
“Ultrasound is useful in PMR {Polymyalgia rheumatica} due to the nature of extra‐articular {around the joint} soft tissue involvement. The most common findings are inflammation and effusion of the subacromial–subdeltoid bursa, biceps tenosynovitis [60, 61], glenohumeral {shoulder} joint inflammation [62] and hip synovitis and trochanteritis [63]. Ultrasound is also useful in ruling out other differential diagnoses such as chondrocalcinosis, early RA {Rheumatoid arthritis} and late‐onset spondyloarthropathy [63] and to be used when screening for large vessel vasculitis and cranial arteritis when these are suspected to coexist with PMR”
“MRI has also been used, although its use is still limited to research purposes in most centres. Typical findings in PMR include a characteristic pattern of symmetrical inflammation in the greater trochanter, acetabulum and ischial tuberosity, reported in 64% of patients with PMR in one study [64]. In another study by Laporte et al., all patients with new‐onset PMR had at least one site of myofascial inflammation, most commonly in the hips, followed by pubic symphysis, shoulders and ischial tuberosity [65]. Advantages of MRI over ultrasound include that MRI is more specific with less interobserver variation in the assessment of vasculitis. However, the disadvantages of MRI include availability, cost and inconvenience for some patients.”
“18‐Fluorodeoxyglucose (FDG) PET CT has been used in oncology and investigation of inflammatory diseases. The uptake of FDG by activated inflammatory cells constitute the basis for using PET CT in PMR and large vessel vasculitis. In patients with suspected PMR, the use of PET CT is not recommended as a routine examination due to limitations such as cost and varying availability. Beside its role in the visualization of inflammation in articular and extra‐articular tissues in PMR, PET CT is extremely helpful in confirming suspected coexistent large vessel vasculitis and differentiation between PMR and other conditions such as malignancies or other rheumatic diseases [66].” Emphasis in bold is mine to highlight this diagnostically useful test that is not recommended because of cost and lack of availability.
(Lundberg et. al, 2022)
Organized Autoimmunity
(Alternative Autoimmune Disease Classification: FIEM, MIEM or BIEM, or FEM, MEM or BEM)
sex predominance (is an autoimmune disease primarily found in genetic Females, Males, or equally in Both?)
Female (Lundberg et. al report female predominance citing Michet & Matteson. Michet & Matteson report 75% female predominance, but do not attribute that number to study sources. Devauchelle-Pensec et. al, in their randomized clinical drug trial, studied 101 participants with Polymyalgia rheumatica; 67.3% were female. Falsetti et. al studied 58 participants with Polymyalgia rheumatica; 60% were female.)
Inherited and acquired gene variations that cause increased susceptibility
Human Leukocyte Antigen (HLA) Associations
HLA-DRB1*13:01, scant evidence suggests a possible link to the development of Polymyalgia rheumatica and/or Giant cell arteritis after influenza vaccination (Liozon et. al, 2021)
HLA-DRB1*0401 and *0404 (Haworth et. al, 1996)
Other Gene Variations (mutations)
(Carvajal et. al, 2020)
Gene Triggering Environmental Exposures
Infections
COVID-19 (Metyas et. al, 2022) (Chang et. al, 2023, found a significantly higher risk of Polymyalgia rheumatica following COVID-19 infection in a study of 3,814,479 participants)
Influenza (Falsetti et. al, 2020 studied a patient-reported correlation, but did not note laboratory confirmation; also cited 6 studies noting influenza infection/vaccination prior to development of Polymyalgia rheumatica symptoms, but most are case series with small numbers of participants)
Drugs
COVID-19 vaccination (Mettler et. al found that COVID-19 vaccination had a lower adverse event reporting profile to influenza vaccination, as it concerns post-vaccination reports of Polymyalgia rheumatica. Out of 1,295 ,482 adverse events reported with COVID-19 vaccination, 290 post-vaccination cases of Polymyalgia rheumatica were reported and 9 cases of Polymyalgia rheumatica together with Giant cell arteritis were reported.)
Influenza vaccination (Mettler et. al found that out of 317,687 adverse events reported with influenza vaccination, 303 post-vaccination cases of Polymyalgia rheumatica were reported and 14 cases of Polymyalgia rheumatica together with Giant cell arteritis were reported.)
Toxins
Not studied.
Stress
Needs to be assessed for each patient
Multiple interactive and destructive immune system pathologies
Elevated Interleukin-6 (Roche et. al, 1996)
“circulating levels of the soluble IL‐6 receptor have been shown to predict future relapses in patients with PMR [33]” (Lundberg et. al, 2022)
(Carvajal et. al, 2020)
Tissue-Type or Cell-Type Attacked
Inflammation and the escape of fluid (effusion) in the subacromial–subdeltoid bursa (fluid-filled sac near the joint)
biceps tenosynovitis
glenohumeral (shoulder) joint inflammation
hip synovitis, and/or muscle inflammation
pubic symphysis inflammation
symmetrical inflammation of the trochanter bone, acetabulum and ischial tuberosity
inflammation of the lining of the arteries
(Lundberg et. al, 2022)
Treatment(s)
The American College of Rheumatology and the European League Against Rheumatism published the following treatment algorithm and guidelines in 2015:
GC = glucorticoids, also known as steroids; NSAIDs = non-steroidal anti-inflammatory drugs; PMR = Polymyalgia rheumatica; MTX = methotrexate; TNFa = Tumor necrosis factor alpha
(Dejaco et. al, 2015)
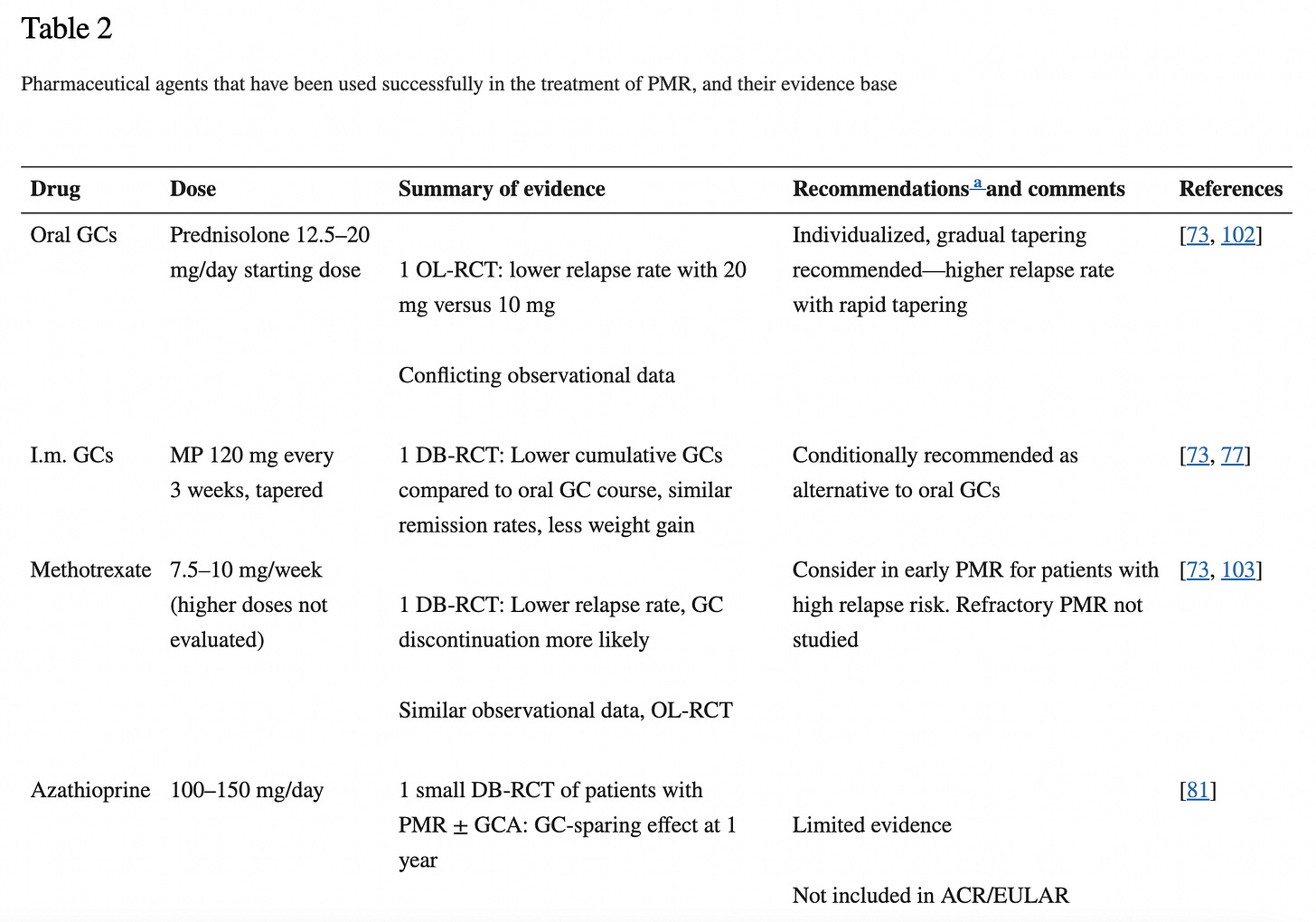
Lundberg et. al created a handy table summarizing the studies to date on different medication treatments for Polymyalgia rheumatica. Some of the evidence is very preliminary and/or low quality:
(2022)
Managing Specialist(s)
Primary care provider (Internist, Family medicine physician, adult medicine physician)
Rheumatologist
Research Authors
Coming Soon
Research Institutions
Coming Soon
Average Time from Symptom Onset to Diagnosis
Not well studied.
Last Updated
September 05, 2023
References
Carvajal Alegria G, Boukhlal S, Cornec D, Devauchelle-Pensec V. The pathophysiology of polymyalgia rheumatica, small pieces of a big puzzle. Autoimmun Rev. 2020 Nov;19(11):102670. doi: 10.1016/j.autrev.2020.102670. Epub 2020 Sep 15. PMID: 32942037.
Chang R, Yen-Ting Chen T, Wang SI, Hung YM, Chen HY, Wei CJ. Risk of autoimmune diseases in patients with COVID-19: A retrospective cohort study. EClinicalMedicine. 2023 Feb;56:101783. doi: 10.1016/j.eclinm.2022.101783. Epub 2023 Jan 10. PMID: 36643619; PMCID: PMC9830133.
Dasgupta B, Cimmino MA, Kremers HM, Schmidt WA, Schirmer M, Salvarani C, Bachta A, Dejaco C, Duftner C, Jensen HS, Duhaut P, Poór G, Kaposi NP, Mandl P, Balint PV, Schmidt Z, Iagnocco A, Nannini C, Cantini F, Macchioni P, Pipitone N, Del Amo M, Espígol-Frigolé G, Cid MC, Martínez-Taboada VM, Nordborg E, Direskeneli H, Aydin SZ, Ahmed K, Hazleman B, Silverman B, Pease C, Wakefield RJ, Luqmani R, Abril A, Michet CJ, Marcus R, Gonter NJ, Maz M, Carter RE, Crowson CS, Matteson EL. 2012 Provisional classification criteria for polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheum. 2012 Apr;64(4):943-54. doi: 10.1002/art.34356. PMID: 22389040.
Dejaco C, Singh YP, Perel P, Hutchings A, Camellino D, Mackie S, Abril A, Bachta A, Balint P, Barraclough K, Bianconi L, Buttgereit F, Carsons S, Ching D, Cid M, Cimmino M, Diamantopoulos A, Docken W, Duftner C, Fashanu B, Gilbert K, Hildreth P, Hollywood J, Jayne D, Lima M, Maharaj A, Mallen C, Martinez-Taboada V, Maz M, Merry S, Miller J, Mori S, Neill L, Nordborg E, Nott J, Padbury H, Pease C, Salvarani C, Schirmer M, Schmidt W, Spiera R, Tronnier D, Wagner A, Whitlock M, Matteson EL, Dasgupta B; European League Against Rheumatism; American College of Rheumatology. 2015 recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Arthritis Rheumatol. 2015 Oct;67(10):2569-80. doi: 10.1002/art.39333. PMID: 26352874.
Devauchelle-Pensec V, Carvajal-Alegria G, Dernis E, Richez C, Truchetet ME, Wendling D, Toussirot E, Perdriger A, Gottenberg JE, Felten R, Fautrel BJ, Chiche L, Hilliquin P, Le Henaff C, Dervieux B, Direz G, Chary-Valckenaere I, Cornec D, Guellec D, Marhadour T, Nowak E, Saraux A. Effect of Tocilizumab on Disease Activity in Patients With Active Polymyalgia Rheumatica Receiving Glucocorticoid Therapy: A Randomized Clinical Trial. JAMA. 2022 Sep 20;328(11):1053-1062. doi: 10.1001/jama.2022.15459. PMID: 36125471.
Falsetti P, Conticini E, Acciai C, Baldi C, Bardelli M, Gentileschi S, Cantarini L, Frediani B. Polymyalgia rheumatica following infective triggers or vaccinations: a different subset of disease? Reumatologia. 2020;58(2):76-80. doi: 10.5114/reum.2020.95360. Epub 2020 Apr 30. PMID: 32476679; PMCID: PMC7249527.
Fors C, Bergström U, Willim M, Pilman E, Turesson C. Validity of polymyalgia rheumatica diagnoses and classification criteria in primary health care. Rheumatol Adv Pract. 2019 Aug 27;3(2):rkz033. doi: 10.1093/rap/rkz033. PMID: 31660474; PMCID: PMC6799851.
Haworth S, Ridgeway J, Stewart I, Dyer PA, Pepper L, Ollier W. Polymyalgia rheumatica is associated with both HLA-DRB1*0401 and DRB1*0404. Br J Rheumatol. 1996 Jul;35(7):632-5. doi: 10.1093/rheumatology/35.7.632. PMID: 8670595.
Liozon E, Parreau S, Filloux M, Dumonteil S, Gondran G, Bezanahary H, Ly KH, Fauchais AL. Giant cell arteritis or polymyalgia rheumatica after influenza vaccination: A study of 12 patients and a literature review. Autoimmun Rev. 2021 Feb;20(2):102732. doi: 10.1016/j.autrev.2020.102732. Epub 2020 Dec 14. PMID: 33326851.
Lundberg IE, Sharma A, Turesson C, Mohammad AJ. An update on polymyalgia rheumatica. J Intern Med. 2022 Nov;292(5):717-732. doi: 10.1111/joim.13525. Epub 2022 Jun 11. PMID: 35612524; PMCID: PMC9796644.
Mettler C, Jonville-Bera AP, Grandvuillemin A, Treluyer JM, Terrier B, Chouchana L. Risk of giant cell arteritis and polymyalgia rheumatica following COVID-19 vaccination: a global pharmacovigilance study. Rheumatology (Oxford). 2022 Feb 2;61(2):865-867. doi: 10.1093/rheumatology/keab756. PMID: 34626105.
Metyas S, Chen C, Aung T, Ballester A, Cheav S. Rheumatologic Manifestations of Post SARS-CoV-2 Infection: A Case Series. Curr Rheumatol Rev. 2022;18(4):346-351. doi: 10.2174/1573397118666220211155716. PMID: 35152867.
Michet CJ, Matteson EL. Polymyalgia rheumatica. BMJ. 2008 Apr 5;336(7647):765-9. doi: 10.1136/bmj.39514.653588.80. PMID: 18390527; PMCID: PMC2287267.
Polymyalgia rheumatica. Autoimmune Association. (2023, April 20). Retrieved June 29, 2023, from https://autoimmune.org/disease-information/polymyalgia-rheumatica/
Polymyalgia rheumatica. Global Autoimmune Institute. (2023). Retrived June 29, 2023, from https://www.autoimmuneinstitute.org/autoimmune-resources/autoimmune-diseases-list/polymyalgia-rheumatica/
Roche NE, Fulbright JW, Wagner AD, Hunder GG, Goronzy JJ, Weyand CM. Correlation of interleukin‐6 production and disease activity in polymyalgia rheumatica and giant cell arteritis. Arthritis Rheum. 1993;36:1286–94