Summary
Postorgasmic illness syndrome (POIS) is a rare condition in which a person develops flu-like and allergy symptoms after orgasm, whether with a partner, through masturbation, or spontaneously during sleep. POIS typically is reported in males (after ejaculation), but females have rarely been reported to have symptoms of POIS. Symptoms may develop within seconds, minutes, or hours after orgasm, and usually last for 2 to 7 days before going away on their own. Possible symptoms vary from person to person, but more common symptoms include fatigue, weakness, headache, fever, mood changes, memory or concentration problems, stuffy nose, sore throat, and itching eyes. The underlying cause of POIS is not known. Some scientists believe that in men, it is an autoimmune or allergic disorder that causes an inflammatory reaction to a substance in a man's own semen. Others have proposed POIS may be caused by a chemical imbalance in the brain. POIS can cause severe distress in people with the condition and their partners. Some people with POIS abstain from sexual activity or find that they need to schedule sex for a time when they can cope with the symptoms.
(Genetic and Rare Diseases Information Center, 2023)
Symptoms
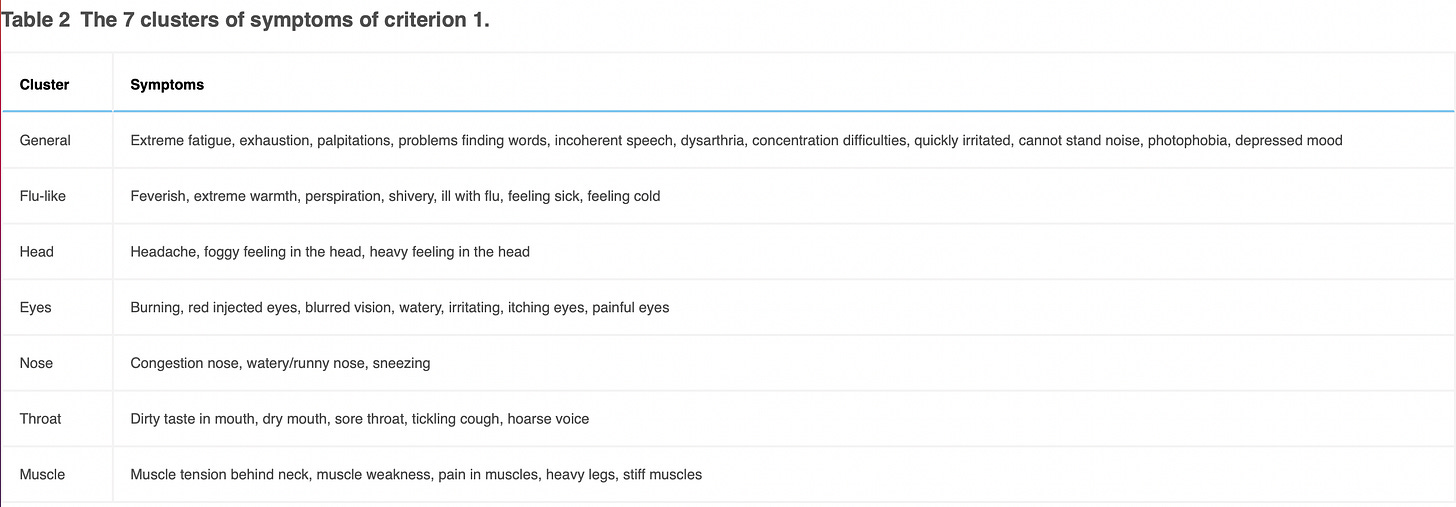
(Waldinger et. al, 2011)
Diagnostic Criteria
It is unclear whether the following criteria is meant for diagnostic or study purposes, or both. Preliminary criteria proposed by Waldinger et. al in 2011:
Study Classification Criteria
See Diagnostic Criteria
Diagnostic Tests
Physical exam to check for inflammation of the epididymis. Surgical removal may be warranted. (Huang et. al, 2022)
a thorough history and physical examination with routine (non-specific to Postorgasmic illness syndrome) tests, including
complete blood count
serum electrolytes
kidney and liver function
sex hormone levels (follicle- stimulating hormone, luteinizing hormone, testosterone)
urine studies
skin prick testing
(Zizzo et. al, 2022)
Organized Autoimmunity
(Alternative Autoimmune Disease Classification: FIEM, MIEM or BIEM, or FEM, MEM or BEM)
sex predominance (is an autoimmune disease primarily found in genetic Females, Males, or equally in Both?)
Male
Inherited and acquired gene variations that cause increased susceptibility
Human Leukocyte Antigen (HLA) Associations
Unstudied
Other Gene Variations (mutations)
Unstudied
Gene Triggering Environmental Exposures
Infections
Unstudied
Toxins
Unstudied
Stress
Needs to be assessed for each patient
Multiple interactive and destructive immune system pathologies
One case study of a single patient, that included three healthy controls for comparison, found no evidence of IgE antibodies in response to exposure to the patient’s own semen. This finding suggests postorgasmic illness syndrome is not an allergic response (Jiang et. al, 2015)
One case study found IgE antibodies in its single patient, that reacted with the patient’s own semen. This finding suggests postorgasmic illness syndrome is an allergic response (Kim et. al, 2018)
3 study subjects lacked evidence of Mast cell activation (an important marker of allergic response) when given a skin prick test with their own semen (Rosetti et. al, 2023)
Tissue-Type or Cell-Type Attacked
Difficult to establish based on current level of research.
Treatment(s)
Hyposensitization treatment
Waldinger used under-the-skin injections of a participants own semen to gradually reduce symptoms of Postorgasmic illness syndrome. Multiple, small exposures over time are a way to reduce reactivity, and is a method used to desensitize patients to a number of different allergens. In Waldinger’s study of two patients, injections were administered every two weeks in the first year, then spaced to every four weeks in the second and third year. The results are so limited by the study size, and design, that it’s hard to draw very many conclusions from his result. He did find a slow reduction of complaints, with 60% improvement in symptoms after 31 months of injections in one participant, and 90% improvement in symptoms after 15 months of injections. The patient experience in all of this was likely to be difficult. To get the semen, the participants would have to expose themselves to the potential for Postorgasmic illness syndrome symptoms every two weeks for a year, then every four weeks for subsequent years. There is the minor pain and inconvenience of the injections, the long time frame, and the incomplete symptom improvement to consider.
(Waldinger et. al, 2011)
Intralymphatic Immunotherapy
Based on a case study (one patient) only. Kim et. al injected the patient’s own semen into an inguinal (groin) lymph node on a monthly basis, for a total of 5 injections. Interestingly, this patient had semen-specific IgE (immune protein E). They note a marked improvement in the patient’s symptoms, and some lab values, although the treatment resulted in flu-like symptoms following the third and fourth injections that persisted for weeks. At 8- and 15-month follow up, after the first injection, sore throat and urinary symptoms were still present, but their duration was shortened. All other Postorgasmic illness syndrome symptoms had resolved.
(Kim et. al, 2018)
Managing Specialist(s)
Urologist
Research Authors
Canada
Leah Rosetti (Department of Psychiatry, University of British Columbia, Vancouver, BC, Canada)
Amin Kanani (Division of Allergy and Immunology, Department of Medicine, University of British Columbia, St. Paul's Hospital, Vancouver, BC, Canada)
Luke Witherspoon (Department of Urologic Sciences, University of British Columbia, Vancouver General Hospital, Vancouver, Canada and Department of Urology, The Ottawa Hospital, Ottawa, BC, Canada)
Ryan Flannigan (Department of Urologic Sciences, University of British Columbia, Vancouver General Hospital, Vancouver, BC, Canada and Department of Urology, Weill Cornell Medicine, New York, NY, United States)
Stacy Elliott (Department of Psychiatry, University of British Columbia, Vancouver, BC, Canada and Department of Urologic Sciences, University of British Columbia, Vancouver General Hospital, Vancouver, BC, Canada and GF Strong Rehabilitation Centre, Vancouver, BC, Canada)
China
Tian-Bao Huang (Department of Urology, Northern Jiangsu People's Hospital and Department of Urology, College of Clinical Medicine, Yangzhou University, Yangzhou 225001, China)
Jun-Jie Yu (Department of Urology, Northern Jiangsu People's Hospital and Department of Urology, College of Clinical Medicine, Yangzhou University, Yangzhou 225001, China)
Yong-Jun Du (Department of Urology, Northern Jiangsu People's Hospital and Department of Urology, College of Clinical Medicine, Yangzhou University, Yangzhou 225001, China)
Zhi-Yong Liu (Department of Urology, Shanghai Changhai Hospital, Second Military Medical University, Shanghai 200433, China)
United States
Caleb Natale (Department of Urology, Tulane University School of Medicine, New Orleans, LA, USA)
Andrew Gabrielson (Johns Hopkins School of Medicine, James Buchanan Brady Urological Institute, Baltimore, MD, USA)
Hoang Minh Tue Nguyen (Department of Urology, Tulane University School of Medicine, New Orleans, LA, USA)
Brian Dick (Department of Urology, Tulane University School of Medicine, New Orleans, LA, USA)
Wayne J G Hellstrom (Department of Urology, Tulane University School of Medicine, New Orleans, LA, USA)
Mark R. Paulos The Men’s Health Center, Miriam Hospital, Warren Alpert Medical School of Brown University, Providence, Rhode Island
Division of Urology, Warren Alpert Medical School of Brown University, Providence, Rhode Island
John Zizzo (Desai Sethi Urological Institute, Miller School of Medicine, University of Miami, Miami, FL, USA)
Luís F. Sávio (Desai Sethi Urological Institute, Miller School of Medicine, University of Miami, Miami, FL, USA)
Ranjith Ramasamy (Desai Sethi Urological Institute, Miller School of Medicine, University of Miami, Miami, FL, USA)
Thiago F. N. Lima (Desai Sethi Urological Institute, Miller School of Medicine, University of Miami, Miami, FL, USA)
Research Institutions
Canada
University of British Columbia, Vancouver, BC, Canada
China
Northern Jiangsu People's Hospital, Yangzhou 225001, China
Yangzhou University, Yangzhou 225001, China
Shanghai Changhai Hospital, Second Military Medical University, Shanghai 200433, China
United States
Tulane University School of Medicine, New Orleans, LA, USA
Johns Hopkins School of Medicine, James Buchanan Brady Urological Institute, Baltimore, MD, USA
Department of Urology, Weill Cornell Medicine, New York, NY, United States
Desai Sethi Urological Institute, Miller School of Medicine, University of Miami, Miami, FL, USA
Average Time from Symptom Onset to Diagnosis
Does not appear in the literature to date.
Last Updated
June 02, 2023
References
Huang TB, Yu JJ, Du YJ, Liu ZY. Novel treatment for post-orgasmic illness syndrome: a case report and literature review. Asian J Androl. 2022 May-Jun;24(3):332-334. doi: 10.4103/aja202170. PMID: 34747723; PMCID: PMC9226701.
Jiang M.D., Guangpeng Xi M.D., Hongjun Li PhD., Jia Yin M.D. Post-orgasmic syndrome in a Chinese Man: no proof for IgE mediated allergy to semen. J Sex Med. 2015; 12: 840-845
Kim TB, Shim YS, Lee SM, Son ES, Shim JW, Lee SP. Intralymphatic Immunotherapy With Autologous Semen in a Korean Man With Post-Orgasmic Illness Syndrome. Sex Med. 2018 Jun;6(2):174-179. doi: 10.1016/j.esxm.2017.12.004. Epub 2018 Mar 15. PMID: 29550252; PMCID: PMC5960017.
Postorgasmic illness syndrome. Genetic and Rare Diseases Information Center, National Center for Advancing Translational Sciences, National Institutes of Health. (2023, February). Retrieved May 15, 2023, from https://rarediseases.info.nih.gov/diseases/10809/postorgasmic-illness-syndrome
Rosetti L, Kanani A, Witherspoon L, Flannigan R, Elliott S. Case series: expanding diagnostic markers in postorgasmic illness syndrome. Sex Med. 2023 Mar 2;11(2):qfac021. doi: 10.1093/sexmed/qfac021. PMID: 36910704; PMCID: PMC9985106.
Waldinger M.D., Meinardi M.M., Zwinderman A.H. Postorgasmic illness syndrome (POIS) in 45 Dutch caucasian males: clinical characteristics and evidence for an immunogenic pathogenesis (Part I). J Sex Med. 2011; 8: 1
Zizzo J, F Sávio L, Ramasamy R, F N Lima T. Postorgasmic Illness Syndrome: An Update. Eur Urol Focus. 2023 Jan;9(1):22-24. doi: 10.1016/j.euf.2022.09.016. Epub 2022 Oct 22. PMID: 36283946.