Juvenile Idiopathic Arthritis: A Mini Test Case in Organized Autoimmunity

Ideal: As Few Arrows As Possible Pointing In Consistent Directions
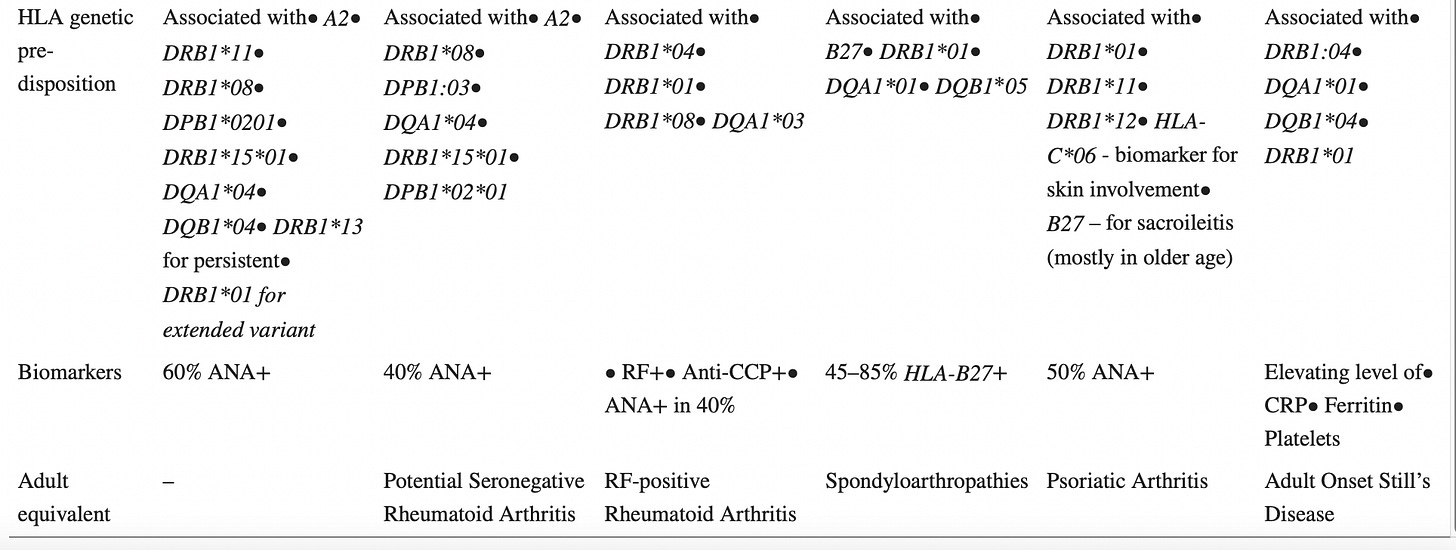
Juvenile idiopathic arthritis, with its numerous sub-types, and robust inventory of scientific evidence, is actually a mini-test case in Organized Autoimmunity. When I say Organized Autoimmunity, I mean classifying and diagnosing autoimmune disease by genetic sex, inherited and acquired gene variations (mutations), environmental exposures and multiple interactive immune system pathologies. And the chart below from the fabulous review article by Zaripova et. al uses the current International League of Associations for Rheumatology criteria to, almost, organize Juvenile idiopathic arthritis for me. You can see at the bottom that there’s plenty of overlap in genetic variations between the different sub-types.
(Zaripova et. al, 2021)
Based on meta-analysis, genetic associations for the sub-types of Juvenile idiopathic arthritis (JIA) can actually be divided between Human Leukocyte Antigen (HLA)-associated sub-types and non-HLA-associated sub-types.
Several studies have documented genetic associations to JIA [21–25]. Genetic linkage depends on subtype and may be divided into two groups: HLA genes and non-HLA-related genes. Meta-analysis of genetic predisposition to JIA subtypes has shown association with HLA class II molecules (A2, DRB1, DPB1) mostly for non-systemic subtypes (Table (Table1),1), while for sJIA the lack of association with HLA genes has been found [21].
(Zaripova et. al, 2021)
This points out the pitfalls of Table 1 above, for including HLA associations for systemic Juvenile idiopathic arthritis that may not have been as extensively evaluated as the meta-analysis referenced above. My practice of including as expansive a list as possible of studied genetic associations has the same pitfall—in the absence of large-scale data, how meaningful are these associations? Nonetheless, I think documenting genetic associations is important, and additional research will help to clarify relevant and irrelevant genetic associations with disease process.
Can researchers eliminate symptomatology, named autoimmune disease and age from their classification criteria?
It would be a big shift, but if research subjects are included in studies according to 1. genetic sex, 2. inherited and acquired gene variations that cause increased disease susceptibility, 3. gene triggering environmental exposures, and 4. multiple interactive and destructive immune system pathologies, then what is lost? Symptomatology, named autoimmune disease, and age-based classifications, which I consider to be more confounding than clarifying. These categories are also less relevant to testing the effectiveness of medication and dietary treatment. So, practically what do I mean? Juvenile idiopathic arthritis, with its evolving study classification criteria provides an excellent example.
For instance, what if Juvenile idiopathic arthritis was divided into separate groups by biological sex, Human Leukocyte Antigen associations, environmental exposures and antibodies. Foundation work would need to be done, including studying the environmental exposures and immune system pathologies of females and males with a pediatrician-diagnosed autoimmune disease and particular HLA-associations. Wait, groups are still divided by age? Reluctantly, yes, because I’m sort of a realist. It would require a systemic overhaul to completely eliminate the pediatric and adult medicine divisions in research. Plus, it’s important to test medications separately in the pediatric population.
Sex Predominance, HLA-B27 and HLA DRB1*08
Interestingly, the International League of Associations for Rheumatology (ILAR) criteria can be roughly re-organized by
female predominance and HLA DRB1*08 (encompasses three out of six ILAR sub-types)
male predominance and HLA-B27 (refers to one ILAR sub-type)
Based on what I’ve read, I’m not even sure it’s worthwhile to consider systemic Juvenile idiopathic arthritis as the same disease as the other sub-types, so I’m mostly ignoring it for the purposes of this post. The Pediatric International Trials Organization (PRINTO) preliminary criteria makes HLA-B27 positivity a criteria for one of its sub-types, flirts with neatly dividing two sub-types by antibody positivity (Anti-nuclear antibody positive for one sub-type, Rheumatoid factor positive for the next sub-type, with a provisional option for anti-cyclic citrullinated protein antibody in place of Rheumatoid factor positivity). PRINTO even eliminated the exclusive requirement of arthritis for systemic Juvenile idiopathic arthritis. I’ve included the PRINTO criteria below.
I went looking for pitfalls in organizing Juvenile idiopathic arthritis by genetic sex and HLA associations, and I can think of many. For example, maybe a male HLA B27 population is too broad to study effectively? According to a study from 2009, it’s actually confined to a relatively small subset of the U.S. population:
Methods: The national prevalence of HLA-B27 was determined as part of the 2009 US National Health and Nutrition Examination Survey (NHANES), a cross-sectional survey monitoring the health and nutritional status of the US civilian, noninstitutionalized population. DNA polymerase chain reaction analysis was conducted in samples from 2,320 adults ages 20-69 years from this nationally representative sample.
Results: The age-adjusted US prevalence of B27 was 6.1% (95% confidence interval [95% CI] 4.6-8.2). By race/ethnicity, the prevalence of B27 was 7.5% (95% CI 5.3-10.4) among non-Hispanic whites and 3.5% (95% CI 2.5-4.8) among all other US races/ethnicities combined. In Mexican Americans, the prevalence was 4.6% (95% CI 3.4-6.1). The prevalence of B27 could not be reliably estimated for other US racial/ethnic groups because of the low number of B27-positive individuals in those groups. For adults 50-69 years of age, the prevalence of B27 was 3.6% (95% CI 2.2-5.8), which suggested a decrease in B27 with age. These prevalence estimates took into account the NHANES survey design and are reviewed with respect to data from the medical literature.
(Reveille et. al, 2012)
I didn’t catch on the first reading that HLA B27 population prevalence decreases with age. Is that due to shorter life expectancy? From factors related to HLA-B27 positivity? Male predominance of HLA-B27 and shorter life expectancy in the male population overall? Both? Neither? Hmmm, a topic for another day.
Zaripova et. al compare the two classifications in this way:
In addition, there is a substantial unclassified cohort of patients with JIA onset before 6 years of age and female predominance having specific features that include symmetric arthritis, iridocyclitis, ANA and HLA-DR8-positivity. In 2019 the Pediatric Rheumatology International Trials Organization (PRINTO) Consensus revised the ILAR classification criteria and proposed to identify this complex of features as early-onset ANA-positive JIA [10]. Other JIA disorders identified according to these preliminary criteria include sJIA, RF-positive JIA and enthesitis/spondylitis-related JIA (Table 2). Arthritis of more than 6 weeks duration that does not fit the criteria is grouped as ‘Other JIA’, and that fitting more than one criterion, ‘unclassified JIA’ [10]. PRINTO Consensus highlights JIA as not a single disease but a group of different disorders, of which diagnosis does not require joint count or the presence of arthritis. The onset of the disease has been changed to before 18 years of age [10].
(Zaripova et. al, 2021)
First off, the Zaripova quote got me thinking about how many people would fall into the “other” category if Juvenile idiopathic arthritis, and all other juvenile autoimmune disease, were classified by genetic sex, HLA associations, environmental exposure and immune pathology. Potentially very few, since people would have at least genetic sex, and HLA or other genetic information, with no proven disease association. A cohort organized in this way might make it easier to find common characteristics, not previously classified. It bothers me that the PRINTO classification uses the term “unclassified JIA.” I would, of course, prefer “Polyautoimmune JIA” or simply Poly-JIA. “Unclassified” is outside of any classification in a way that’s difficult to distinguish from “other.” Poly JIA encompasses the different classes.
Why It Matters
I am sure reading about classification systems is not everybody’s cup of tea, and I know I haven’t fully articulated how Organized Autoimmunity would really function in a research or clinical environment, because I don’t know. I also can’t quite imagine how Organized Autoimmunity divorces itself from named autoimmune disease. Sometimes I think that’s one of its strengths—that it could be used parallel to the body of research on named autoimmune disease. Sometimes I don’t see how it can fully function if it's still tied to the constraints of named autoimmune disease. And none of this hemming and hawing explains why it matters. Accurate classification of disease clarifies rather than confuses. It leads to all the arrows pointing in consistent directions, even if those directions are different, from study to study to study, and clinician to clinician to clinician. Accurate classification criteria, that hopefully leads to accurate diagnostic criteria, focuses assessment on particular kinds of concrete testing, without being as clouded by the biases and subjectivity of clinicians.
This post concludes my look at Juvenile idiopathic arthritis. Next up, is Post-Orgasmic Illness Syndrome. I am working my way through reader-requests for more information and analysis on particular autoimmune diagnoses. If you would like me to take a closer look at a particular diagnosis, please leave a comment below. If you don’t feel comfortable commenting publicly, email me at autoimmunedx@gmail.com
References
Reveille JD, Hirsch R, Dillon CF, Carroll MD, Weisman MH. The prevalence of HLA-B27 in the US: data from the US National Health and Nutrition Examination Survey, 2009. Arthritis Rheum. 2012 May;64(5):1407-11. doi: 10.1002/art.33503. PMID: 22139851; PMCID: PMC4038331.
Zaripova LN, Midgley A, Christmas SE, Beresford MW, Baildam EM, Oldershaw RA. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol Online J. 2021 Aug 23;19(1):135. doi: 10.1186/s12969-021-00629-8. PMID: 34425842; PMCID: PMC8383464.