Kids and Polyautoimmunity

It’s harder for me to write about children and autoimmunity. My personal, and nursing, background with autoimmunity is with adults. As a nurse, I have also worked antepartum, intrapartum and postpartum hospital care. The children I had as patients were either newborns or teenagers, which had its share of tragedy, but mainly focused on the joyous. I have a harder time depersonalizing children to just the numbers they represent, or the interesting aspects a study can reveal about their disease process—individually and in aggregate. I can only guess at why it’s easier for me to depersonalize adults—maybe because I have more practice doing it.
Healthcare propagandists, who are mainly found among the administrative ranks with zero recent patient contact hours, strenuously deny that this is the case, but a certain degree of sociopathy is required for any healthcare worker to get through their day. Objectification, depersonalization, morbid curiosity—these are required behaviors to do something fundamentally painful to someone else, like sewing up a person’s skin; or fundamentally uncomfortable, like checking a patient’s cervical dilation; or fundamentally impolite, like asking probing questions about a person’s bowel movements. With practice, these violations of normal human interactions are easier, especially when you know that what you’re doing is ultimately helpful.
Research on children (and adults) is so challenging, because unlike a medical procedure or evaluation, the research is unlikely to be helpful to the particular children involved, and may only serve to advance scientific knowledge a little bit. Although I find autoimmunity fascinating, and I am compelled by personal and professional experience to learn more, I do see the pain embodied in these studies. I particularly struggle with reading and writing about the studies on children. I justify my insatiable curiosity by reminding myself of what I am trying to do—to review the scientific research on autoimmunity for a general audience, organize what is known about autoimmunity in a more accessible way, and inform and empower autoimmune disease symptom sufferers and their support persons. Please keep reading to learn about children and polyautoimmunity in a rheumatological setting.
Area of Investigation
Multiple Autoimmune Syndrome: when one person meets the study classification criteria for three or more autoimmune diseases.
Study Title
Juvenile polyautoimmunity in a rheumatology setting
Results
313 children with polyautoimmunity, meeting study classification criteria, were included in this Colombian study, which spanned from June 2015 to June 2018. Among others, this study is authored by the Colombian polyautoimmunity expert, and researcher, Juan Manuel Anaya. He has consistently authored, along with a changing group of other authors and institutions, a number of studies that I have reviewed on polyautoimmunity in the last 12 years. More than any other author, his framework for understanding and classifying polyautoimmunity has influenced me the most.
This study’s results revealed that 138 (44%) participants developed two autoimmune diseases simultaneously (less than 6 months apart). The rest developed a second autoimmune disease within approximately 2-3 years. 62 (19.8%) participants had Multiple autoimmune syndrome. The ratio of male to female participants with Multiple autoimmune syndrome was 1(male) to 7.8(females).
55 (17.57%) had siblings or parents with an autoimmune disease. The most common autoimmune diseases reported for parents were Hashimoto’s thyroiditis, Systemic Lupus Erythematosus and Rheumatoid arthritis. The most common autoimmune diseases reported for siblings were Hashimoto’s thyroiditis, Systemic Lupus Erythematosus and Type 1 Diabetes. 52 (16.61%) participants reported autoimmune diseases in extended family members—grandparents, aunts, uncles, and cousins. A history of familial autoimmunity, including close and extended family members, was more common in boys than in girls. This finding makes sense to me, since a greater genetic predilection for autoimmunity may be necessary for boys to develop autoimmunity, given the female predominance of most autoimmune diseases.
Participants with siblings with autoimmunity had an earlier age at onset of the index autoimmune disease than participants with siblings free from autoimmunity. The index autoimmune disease is defined in this study as the first identified autoimmune disease. Participants who had siblings with autoimmune disease had a longer time between diagnosis of the first and second autoimmune disease. These findings make me question whether the onset of the autoimmune disease in these participants was truly earlier, or whether it was recognized and diagnosed sooner because of a greater suspicion of autoimmunity due to a sibling history of autoimmunity.
Simultaneous autoimmune diagnoses (less than 6 months apart) occurred in older participants compared with sequential autoimmune diagnoses (more than 6 months apart). This supports the evidence in other studies that polyautoimmunity tends to develop over time, in children and adults.
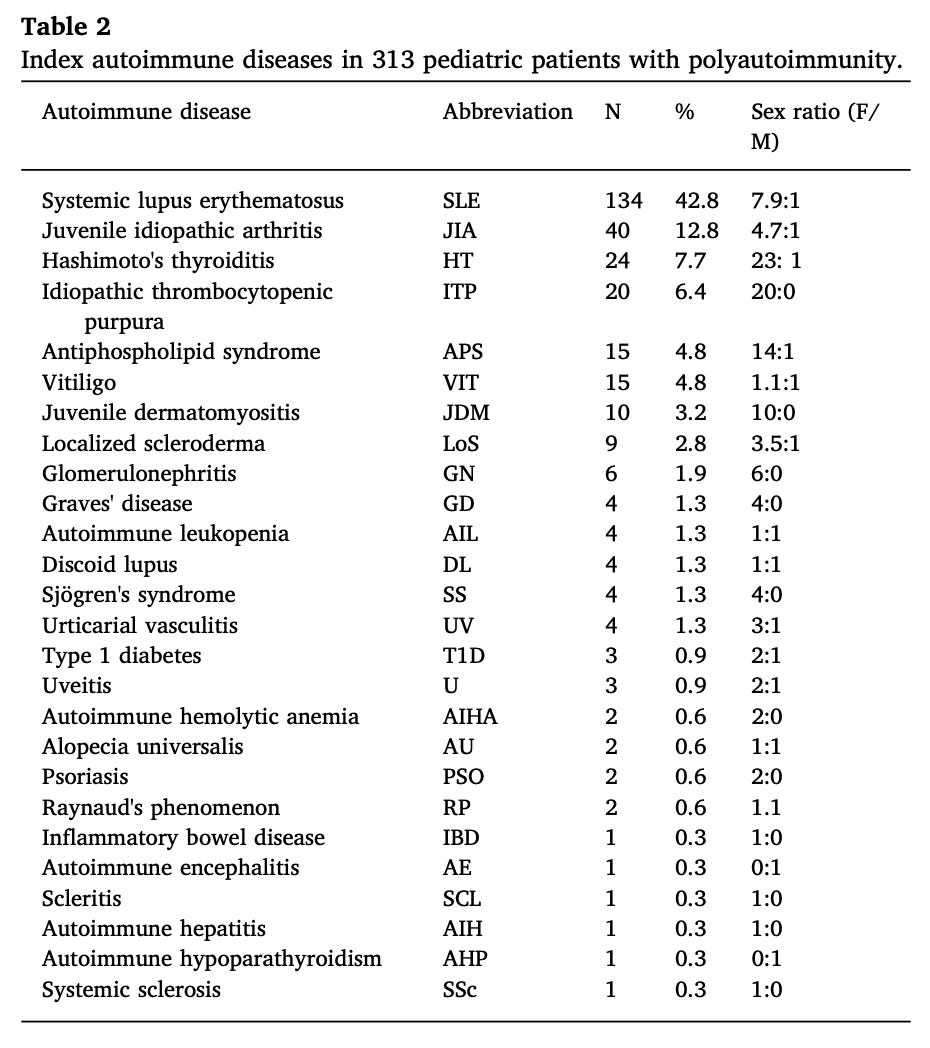
Of the 313 participants, Immune thrombocytopenic purpura (ITP), Graves’ disease, juvenile dermatomyositis and Sjogren’s syndrome were exclusive to girls. The following table breaks down the percentage of participants by index autoimmune disease (first autoimmune disease diagnosed) and the sex ratio of each. N = Number of participants in the study with the autoimmune disease.
There was also a difference in autoimmune disease prevalence based on which decade of life the child was in, the first decade or the second decade. Juvenile idiopathic arthritis, Immune thrombocytopenic purpura, Juvenile dermatomyositis, and Vitiligo, were the most common autoimmune diseases diagnosed in the first decade of life. Systemic Lupus Erythematosus and Antiphospholipid syndrome were the most common autoimmune diagnoses during the second decade of life.
The following graphic illustrates co-occurring autoimmune diseases organized by index autoimmune disease. SLE = Systemic lupus Erythematosus. JIA = Juvenile idiopathic arthritis. HT = Hashimoto’s thyroiditis. ITP = Immune thrombocytopenic purpura. APS = Antiphospholipid syndrome. VIT = vitiligo.
Especially striking to me is the strong, nearly exclusive, association between Systemic Lupus Erythematosus and Antiphospholipid syndrome. This association has been noted in other studies.
Why it Matters
Emphasis added in bold is mine.
Three main clusters of Polyautoimmunity were determined (Fig. 7). The first one involved Systemic Lupus Erythematosus and Antiphospholipid Syndrome. The second one was characterized by Hashimoto’s Thyroiditis, Juvenile Idiopathic Arthritis, Sjogren’s Syndrome, and Immune Thrombocytopenic Purpura, and the third one by Vitiligo and Localized Scleroderma. These clusters represent the most significant combinations of Polyautoimmunity in our series, and may serve to guide the screening of patients for Polyautoimmunity with any of the Autoimmune Dieseases present in the clusters. Those combinations depend upon the prevalence of Autoimmune Diseases, and these may vary from one population to another due to genetic background, ancestry, and environmental factors.
Study Type
For reference, I have ranked medical study types in order of least likely to be affected by hidden bias to most likely to be affected. Those studies that are most likely to be affected by hidden bias should be taken seriously, but not given the same weight as studies that are less likely to be affected by hidden bias. This study’s type appears in bold below.
Clinical Trial
Observational Study
Prospective
Retrospective
Cross-sectional
*Starting next week, I’m changing my posting schedule to Tuesdays and Fridays at 11AM. Mondays appear to be a difficult day for readers to dig into dense content.
References
Malagón C, Gomez MDP, Mosquera C, Vargas C, Gonzalez T, Arango C, Martin L, Perez P, Amaya-Uribe L, Molano-Gonzalez N, Anaya JM. Juvenile polyautoimmunity in a rheumatology setting. Autoimmun Rev. 2019 Apr;18(4):369-381. doi: 10.1016/j.autrev.2018.11.006. Epub 2019 Feb 14. PMID: 30772494.